Mother’s milk has been long touted for its salutary effects on the newborn and its ability to shield infants from certain infections.
Now research from Harvard Medical School conducted in mice shows that at least part of its protective effects come from a surprising source: the microbes residing in maternal intestines.
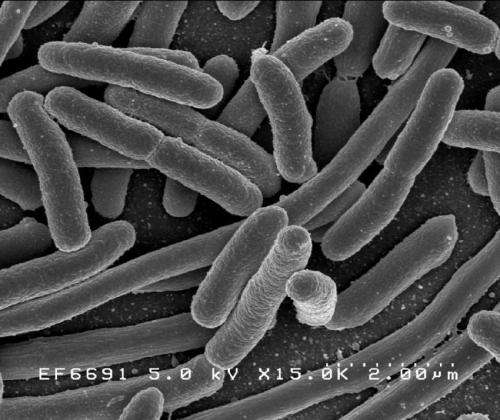
The new study, published Jan. 8 in Nature, shows that antibodies made in response to one particular organism in the maternal gut are passed on to the offspring both via milk and through the placenta to protect newborn pups from infection by at least one disease-causing, and potentially lethal, microbe, E. coli.
The findings add to a growing body of evidence pointing to the potent role of the microbiota—the trillions of microbes that dwell in the gut, skin, mouth and other parts of the bodies of mammals, including humans—in disease and health.
But the new research goes a step further—it specifically identifies maternal microbiota as source of newborn immunity. It further suggests that the intestinal microbiota could offer immune protection even when mothers have had no prior encounters with an infection that allows them to build and pass on protective antibodies to their offspring.
“Our results help explain why newborns are protected from certain disease-causing microbes despite their underdeveloped immune systems and lack of prior encounters with these microbes,” said study senior investigator Dennis Kasper, professor of immunology in the Blavatnik Institute at Harvard Medical School. “Moreover, they raise the possibility that mothers can confer immune protection to their offspring even to pathogens that they haven’t themselves encountered in the past.”
If affirmed through further studies, the findings could inform the design of microbial therapies against dangerous infections such as E. coli and other disease-causing organisms, the researchers said.
“Albeit preliminary, we are hopeful these insights could inform the development of vaccines derived from commensal microbial molecules as a way to prevent infectious diseases,” said Kasper, who is also the William Ellery Channing Professor of Medicine at Brigham and Women’s Hospital. “Another therapeutic avenue could be the use of commensal microbes as probiotics that protect against diarrheal disease.”
Infectious diarrhea—most commonly due to E. coli or rotavirus—is the leading cause of malnutrition and the second leading cause of death globally in children under age 5. It causes 1.7 billion infections and claims more than 520,000 lives a year worldwide, according to the World Health Organization.
Without any prior exposure to microbes, a newborn’s immune system is a blank slate. For the first three weeks, a newborn’s immune protection is derived entirely from maternal antibodies passed onto the fetus during pregnancy via the placenta, during birth via the birth canal, and shortly after birth via breastfeeding.
In the current study, researchers worked with newborn mice genetically engineered to lack B cells—the antibody-producing factories of the immune system. Some of the newborn mice were subsequently raised by mothers that were also born without antibody-making B cells, and therefore, lacked protective antibodies. The other newborn mice were raised by mothers that had normal immune systems.
Mice exposed to protective antibodies from their mothers were far more resistant to E. coli infection than mice that were not exposed to such antibodies. It was as if the pups repelled the pathogen, the researchers observed. Indeed, their intestines had 33 times fewer E. coli bacteria than newborn mice lacking maternal antibodies. By contrast, mice pups that were not exposed to protective antibodies developed disseminated E. coli disease.
The researchers were also able to pinpoint the specific organism responsible for inducing the formation of the protective antibodies—a microbe called Pantoea, member of the Enterobacteriaceae bacterial family, which resides in the intestines of mice and other mammals, including humans.
Source: Read Full Article