To improve the treatment efficacy and overall survival and recovery rates related to severe traumatic brain injury (TBI) in children, 3rd edition of the Brain Trauma Foundation Guidelines for the Management of Pediatric Severe TBI has been issued by a panel of experts in the field of pediatric critical care and neurosurgery.
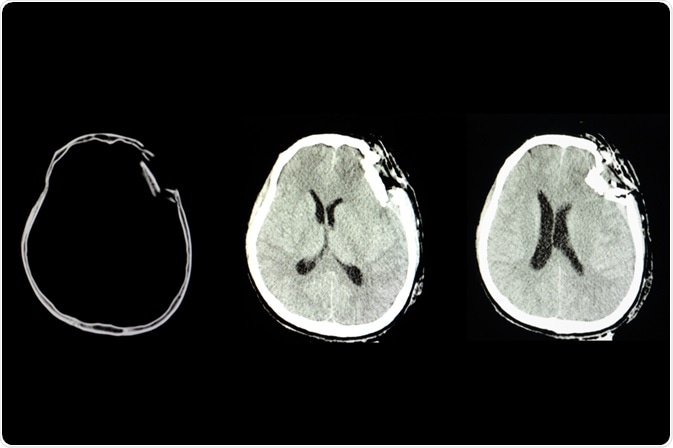
Image Credit: Tomatheart/Shutterstock.com
What is a pediatric traumatic brain injury?
Traumatic brain injury (TBI) mainly occurs due to a sudden bump, blow, or jolt to the head, and the condition is associated with impairment in the brain’s normal activity. It is a leading cause of mortality or permanent disability in children.
Even a small volume of blood loss can induce hemorrhagic shock in children, which makes them highly susceptible to TBI.
In the United States, TBI affects more than 600,000 children every year; of them, approximately 7000 children die and the rest live with chronic health conditions, such as learning impairment, communication difficulties, and seizures.
Although both children and adults share similar symptoms of TBI, the impact is much higher in children because of the developing brain anatomy and age-specific characteristics of the skull, brain, face, and neck muscles.
Regarding causative factors, almost 50% of TBI occur due to falls, and the most vulnerable population are children and elderly people. The second leading cause of TBI is bump by or into an object. In addition, TBI can occur due to car accidents, intentional self-harm, or abusive head trauma.
What does the updated version of severe pediatric TBI guidelines say?
In 2019, the Brain Trauma Foundation has released a newly revised version (3rd edition) of their "Guidelines for the Management of Pediatric Severe Traumatic Brain Injury" for improving the treatment efficacy and recovery and survival rates of children suffering from severe TBI.
The new guidelines include 8 new or revised recommendations for healthcare professionals to improve the treatment quality, and these recommendations are furnished with new information collected from nearly 50 research studies.
A wide variety of information, including utilization of intracranial monitoring system and hypertonic saline-based reduction of acute brain swelling, has been included in the new edition.
As a guide to the recommendations, a treatment algorithm has also been made to guide the use of 1st and 2nd tier treatments for children with severe TBI. The evidence-based studies that are used to make the recommendations are evaluated to create the algorithm. In addition, expert consensus is applied while making the algorithm.
The combination of expert opinions and evidence-based research observations is expected to be helpful for healthcare professionals for treating severe TBI cases.
All the recommendations are clustered into three separate categories: monitoring recommendations, threshold recommendations, and treatment recommendations.
The foundation has also graded (levels I, II, and III) the recommendations according to the evidence quality used to make them. The recommendations that are made from high-quality, moderate-quality, and low-quality evidence are graded as level I, level II, and level III, respectively.
In the new edition, four recommendations, which are graded as level III, are made to improve the efficacy of three types of monitoring systems: intracranial pressure monitoring, advanced cerebral monitoring, and neuroimaging (newly added).
Although monitoring is not directly related to the improvement in patient outcomes, information collected from monitoring can improve treatment efficacy when used in synergy with clinical assessment in taking treatment decisions.
The threshold recommendations are made to suggest threshold values that are used in different monitoring systems. For example, in the case of intracranial pressure monitoring, a target threshold value of less than 20 mmHg is recommended. Similarly, in the case of cerebral perfusion pressure monitoring, a threshold value of 40 mmHg is recommended.
In the treatment category, 15 recommendations are made to cover 10 different treatment strategies. These recommendations are either specific to hospital-based TBI management or associated with risks experienced by children with TBI. About 50% of these recommendations are new or revised.
All recommendations are made to improve important TBI-related treatment options, including hyperosmolar therapy, analgesics, sedatives, and neuromuscular blockade, cerebrospinal fluid drainage, seizure prophylaxis, ventilation therapies, temperature control, barbiturates, decompressive craniectomy, nutrition, and corticosteroids.
Regarding the quality of evidence, the recommendations made for controlling intracranial pressure by hyperosmolar therapy and nutrition and temperature control for overall improvement in treatment outcomes are graded as level II. The rest of the recommendations are graded as level III.
Sources
- CDC. 2019. Basic Information about Traumatic Brain Injury. https://www.cdc.gov/traumaticbraininjury/basics.html
- Science Daily. 2019. Traumatic brain injury and kids: New treatment guidelines issued.https://www.sciencedaily.com/releases/2019/03/190301192651.htm
- AAFP. 2019. New Edition of Severe Pediatric TBI Guidelines Published. https://www.aafp.org/news/health-of-the-public/20190326kidstbi.html
- AAFP. 2019. Pediatric Severe Traumatic Brain Injury Guideline Recommendations by Topic Area and Level of Evidence. www.aafp.org/…/TBI_Guidelines_Recommendations.pdf
Further Reading
- All Traumatic Brain Injury Content
- Quest for an Acute Traumatic Brain Injury Treatment
Last Updated: Apr 15, 2020

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article
