Examining protein changes in peripheral blood cells just 24 hours after initiating chemotherapy for acute myeloid leukemia (AML) could predict 5-year overall survival, potentially allowing treatment to be changed, say Norwegian researchers.
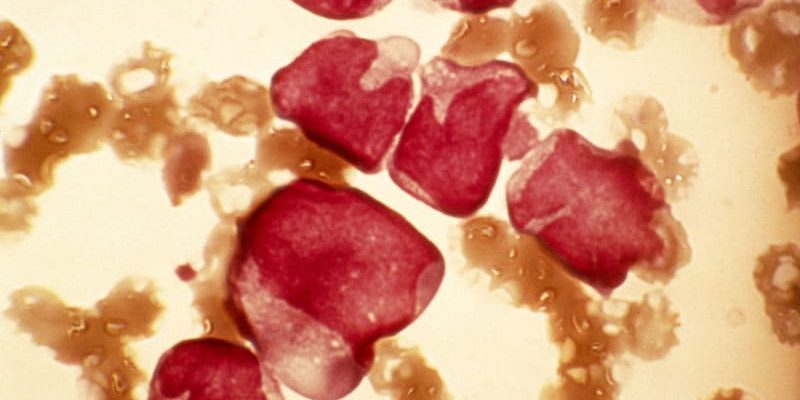
They studied peripheral blood samples from patients with AML and healthy controls, finding that there were several clusters of cells that were different between the two groups, with one cell type expanded only in AML samples.
The results, coreg action published online January 7 in Nature Communications, revealed that patients with high levels of extracellular-signal-regulated kinase (ERK)1/2 in these cells at 24 hours had worse overall survival at both 2 years and 5 years.
“We believe that this protein is responsible for the cancer cells’ resistance to chemotherapy and can be used to distinguish responders from nonresponders,” said first author Benedicte Sjo Tislevoll, PhD Candidate, Centre for Cancer Biomarkers, Department of Clinical Science, University of Bergen, Bergen, Norway, in a statement.
She added: “We think that this is an important key in our understanding of cancer, and our aim is to use this information to change treatment early for patients who are not responding to therapy.”
Study Details
AML is characterized by having numerous genetic aberrations and poor overall survival, the researchers say. Standard treatment for newly diagnosed fit patients is combination chemotherapy with an anthracycline and cytarabine.
While initial remission rates can reach as high as 80%, relapse is a “challenge” in over 40% of patients. It is estimated that up to 60% of patients with AML harbor mutations in signal transduction pathways, and changes in gene expression have been noted “within hours” of starting chemotherapy, including in those regulating cell death and survival.
Yet “when treating patients with leukemia, it is challenging to quickly follow if the patient is responding to therapy or not,” said Tislevoll.
Tools to facilitate the early detection of responders and nonresponders “will be essential to improve cancer patient survival,” by providing physicians with “patient-specific information to change treatment strategy early and avoid unnecessary adverse effects,” the authors comment.
As the intratumor heterogeneity of AML underlines the needs of single-cell resolution, the researchers used mass spectrometry to study peripheral blood samples from 32 patients newly diagnosed with the disease who had started standardized induction chemotherapy in the previous 24 hours.
Samples were taken immediately before, 4 hours after, and 24 hours after the start of chemotherapy. In addition, four peripheral blood samples and three bone marrow samples from healthy volunteers were used as reference samples, and peripheral blood samples from a further seven healthy donors were used as a control group.
The samples were processed with 20 minutes of being taken in order to preserve the intracellular signaling networks, and were then stained with an antibody panel of 21 surface and 15 intracellular markers.
The median age of the patients was 56.3 years; 19 were male, 13 female.
Analyzing the peripheral blood samples, the researchers identified 10 metaclusters of cells that could differentiate the major healthy cell populations from AML blast cells. One of these, MC9, had a myeloid phenotype and was expanded in all AML patients and in the bone marrow of healthy individuals, but not in healthy peripheral blood.
A LASSO Cox regression model revealed that levels of phosphorylated (p-)ERK1/2 at 24 hours in MC9 cells was the most significant predictor of 2-year overall survival (adjusted P = .0004), and five-year overall survival (adjusted P = .0003).
Splitting the patient cohort by median p-ERK1/2 levels at 24 hours, the team found that patients with a high level in MC9 cells had significantly worse 2-year (P = .0048) and 5-year overall survival (P = .0015) than those with levels below the median.
A further Cox regression analysis taking into account European Leukemia Net 2017 risk classification, age, white blood cell count at the time of diagnosis, and allogeneic stem cell transplantation showed that peripheral ERK1/2 levels at 24 hours in MC9 cells were the only predictive marker for 5-year overall survival (P = .000581).
Interestingly, the degree of reduction in peripheral ERK1/2 levels between pretreatment assessment and 24 hours after starting chemotherapy was also predictive of 5-year overall survival (P = .0333).
The researchers also found that the second-most important marker was the level of p38 mitogen-activated protein kinase (MAPK) phosphorylation in MC9 cells 24 hours post-chemotherapy initiation, predicting both 2-year (adjusted P = .0013) and 5-year overall survival (adjusted P = .0005).
Further study showed that patients with high p-ERK1/2 levels 24 hours post-chemotherapy initiation had induction of MAPK target gene expression, alongside an increase in the p38 target MAPK activated protein kinase 2.
The study was supported by grants provided by EU ERA PerMed AML_PM, the Research Council of Norway, the Norwegian Cancer Society with Solveig & Ole Lunds Legacy, Øyvinn M ø lbach-Petersens Fund for Clinical Research, Western Norway Health Authorities, and Norwegian Health Authority South-East. It was partly supported by the Research Council of Norway through its Centres of the Excellence funding scheme. The authors report no relevant financial relationships.
Nat Commun. Published online January 7, 2023. Full text
For more from Medscape Oncology, join us on Twitter and Facebook
Source: Read Full Article