For transgender or nonbinary patients, the obstacles of accessing medical care often begin as soon as they enter their doctor’s office. While many patients may not think twice about sex- or gender-related questions as they fill out patient intake forms in the waiting room, for the more than 1 million transgender individuals living in the United States alone, answering questions such as these can be challenging—especially when these forms include outdated or discriminatory language.
Sexual orientation and gender identity (SOGI) data collection policies are often put into place in healthcare settings without sufficient knowledge about meeting the needs of transgender patients, according to Clair Kronk, Ph.D., postdoctoral fellow in medical informatics. To address common biases in electronic health records (EHR) systems, transgender researchers from institutions across the United States and Canada came together with Kronk as lead author to publish a paper in the Journal of the American Medical Informatics Association. outlined their recommendations for improving EHR data representation in a way that improves transgender patients’ experience as well as gender-diverse research.
“This is the first time that 17 trans authors got together and said, ‘This is what we want and what we need,'” says Kronk. “A lot of the current standards and recommendations may have only one transgender author. But the whole paradigm of research should be ‘nothing about us without us.'”
About a third of transgender patients have reported negative interactions with their medical providers, and fear of mistreatment deters 23% from seeking care, according to a survey by the National Center for Transgender Equality. Transgender individuals have cited misgendering, pathologization, and other forms of discrimination as reasons for avoiding their doctor’s office. For example, discriminatory terms such as “sodomy,” “transvestic fetishism,” and “transsexual syndrome,” the authors report, are still used by some medical professionals. Furthermore, they continue, despite many transgender people being neurodiverse, it is not uncommon for other transgender patients to have their transness itself characterized as schizophrenia, borderline personality disorder, autism, or other disorders.
To address forms of discrimination that persist in electronic health records, Kronk’s team conducted an in-depth literature review and presented recommendations for improving SOGI data collection.
“Implementing these recommendations will allow for more individualized care on a patient level that is not only affirming, but also in line with current research for best practices and standards of care,” says Kronk.
In a 2018 study surveying 365 Canadian medical schools, only 6% of medical students reported feeling that they had adequate knowledge relating to transgender care. Due to this stark lack of knowledge across medical communities, many providers aren’t aware of how to ask for a patient’s gender identity. Outdated terms such as “MTF” (male-to-female), “FTM” (female-to-male), and “transgender male/female, are still frequently used in EHR systems. Furthermore, the inclusion of an “other” category on patient forms is exclusionary language that may alienate transgender or nonbinary individuals.
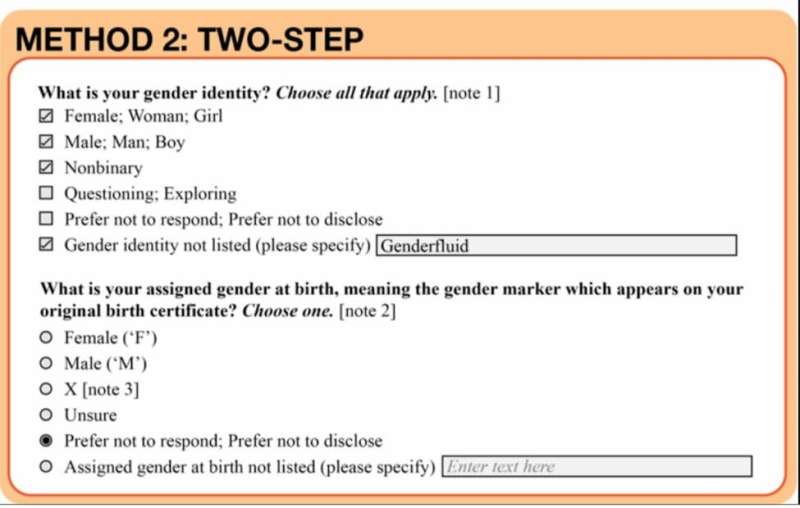
Instead, the authors call for the American Medical Informatics Association and its members to endorse a two-step self-identification approach when collecting data related to a patient’s SOGI. This method (see figure) allows individuals to specify both their gender identity—female, male, nonbinary, questioning, not listed, or prefer not to disclose—and their assigned gender at birth, or the gender that appears on their birth certificate. This approach, the authors say, not only validates patients’ identities, but also allows for more thorough and accurate data analytics.
“We can’t do clinical trials if we’re not setting up groups correctly,” says Kronk. “This method will lead to easier cohort construction for research.” Furthermore, the two-step method, the authors write, has been recommended by multiple prominent institutions, including the UCSF Center of Excellence for Transgender Health, Fenway Health in Boston, the Mayo Clinic, and the U.S. Centers for Disease Control and Prevention.
In addition to endorsing the two-step method, the authors also examine the benefits and pitfalls of karyotyping and organ inventories—processes used to examine patients’ chromosomes and better understand their anatomy, respectively. While there are cases in which taking these measures can provide important health information, they are not always medically necessary. The authors call for more research into the ethical implementation of both of these processes.
Ultimately, says Kronk, taking these steps is simply a starting point for optimizing care for transgender and other marginalized patients. Last year, she was eliminated from a COVID-19 vaccine trial after disclosing her status as transgender. But how, she asks, can providers provide equitable care for transgender and nonbinary individuals when they are being excluded from medical research? Kronk hopes that her team’s recommendations will help promote greater representation of diverse groups in clinical trials.
Source: Read Full Article
