T cells are a part of the immune system that focuses on specific foreign particles. Rather than generically attack any antigens, T cells circulate until they encounter their specific antigen. As such, T cells play a critical part in immunity to foreign substances.
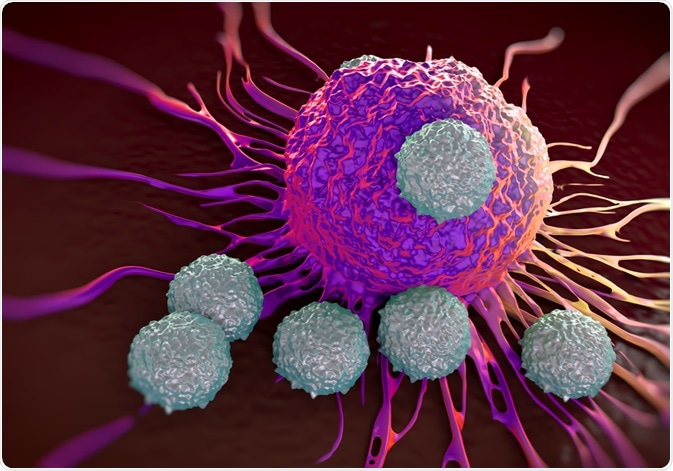
Image Credit: royaltystockphoto.com/Shutterstock.com
T cell function and use
The most common context of T cells is within infectious diseases, but they are used for other aspects of adaptive immunity too. This includes responses to allergens and tumors. They maintain immune homeostasis in humans over decades, but can also be responsible for inflammatory or autoimmune diseases.
The role of T cells is slightly modified throughout the human lifetime. In infancy, naïve T cells are critical for developing immunity towards common pathogens or antigens. During this time, long-term reserves of memory T cells are established and can be maintained through adulthood.
In adulthood, when fewer novel antigens are encountered, they function mainly to maintain homeostasis and immunoregulation of repeat or chronically encountered antigens. There is also some focus on surveillance for tumors during this stage in life.
Later in life, the functionality of T cells decreases, which adds to the dysregulation of the immune system and associated pathologies.
T cell activation and mechanism
T cells originate in the bone marrow but are matured in the thymus. However, they are not activated until they find their specific antigen. They bind to this antigen on the surface of antigen-presenting cells (APCs). Typically, several types of T cells are involved in this, mainly CD4 helper T cells and CD8 cytotoxic T cells, and together they form the MHC complex.
The activation of T cells is not always as binding to the MHC. Both helper T cells and cytotoxic T cells (two of the types of T cells) need secondary signals to become fully activated and be effective towards the threat. These are provided by several molecules, such as CD28 which activate helper T cells.
In general, there are three types of T cells: cytotoxic, helper, and regulatory. All of these must react to foreign antigens strongly to be effective for immunity. T cells with a strong reaction are also given survival signals by several molecules, such as ICOS and OX40. These are only expressed on the T cell surface following binding with the antigen, to ensure it is only active after response to a pathogen.
After activation, communication occurs in the form of cytokines. The cytokines decide what form of responder the cells turn into. Helper T cells become Th1, Th2, or IL-17 types. Each of these types has its own role in the continued development of further immune responses.
T cells and COVID-19
Because the clearing of a virus depends on an effective immune response, T cells have again come into focus following the COVID-19 pandemic. Therefore, boosting the function and quantity of T cells is important in COVID-19 patients to ensure recovery.
While the research is so far limited, initial studies indicate that there is a decrease in T cells in patients with COVID-19. This is also related to the severity of the disease, with 70.56% of non-ICU patients having decreased levels of total T cells, CD4 and CD8 T cells. ICU patients had even higher, with 95% of patients showing a decrease in total T cells and CD4 T cells. 100% of ICU patients also had decreased CD8 T cell levels.
However, the mechanism of this is still uncertain. There is some hypothesis that this is an artifact of the age groups commonly hospitalized for COVID-19 – people over the age of 60, who are disproportionately hospitalized, can be experiencing reduced T cell levels due to higher levels of cytokines such as TNF-α and IL-10. Dysregulated cytokine levels can be central in cases of chronic inflammation.
There is also some evidence that deleterious progression of COVID can be prevented in patients with low T cell counts. Because of the suspected role of cytokines, blocking these can potentially be an effective strategy to prevent T cell exhaustion and allow for more positive COVID-19 outcomes.
Some cytokines, or some of these such as IL-10, are inhibitory cytokines and as such, they can prevent T cell proliferation. This means their elevated presence in COVID-19 patients can be central to the observed reduced levels of T cells and can be linked to poorer COVID-19 outcomes.
Image Credit: sciencepics/Shutterstock.com
Sources
- Cavanagh, M., and Gwyer Findlay, E., 2020. T Cell Activation. [online] Immunology.org. Available at: <https://www.immunology.org/public-information/bitesized-immunology/systems-and-processes/t-cell-activation>
- Kumar, B., Connors, T., and Farber, D., 2018. Human T Cell Development, Localization, and Function throughout Life. Immunity, 48(2), pp.202-213.
- Diao, B., Wang, C., Tan, Y., Chen, X., Liu, Y., Ning, L., Chen, L., Li, M., Liu, Y., Wang, G., Yuan, Z., Feng, Z., Zhang, Y., Wu, Y. and Chen, Y., 2020. Reduction and Functional Exhaustion of T Cells in Patients with Coronavirus Disease 2019 (COVID-19). Frontiers in Immunology, 11.
Last Updated: Jun 17, 2020

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article
