Skip to:
- The endogenous opioid system
- What roles does the system play?
- Endogenous opioids and addiction
- Post-operative pain and endogenous endorphins
Before scientists discovered endogenous opioids in the 1970s, opioids were only understood in terms of the effects that opioid drugs have, such as inducing sleep, relieving pain, and causing addiction.
After studying various opium extracts, scientists started to realize that the differential effects that they would have must be accounted for by the presence of endogenous opioid receptors. This led them to begin searching for endogenous opioid ligands and the receptors they bind to.
The endogenous opioid system
Since then, researchers have discovered the endogenous opioid system and its significance in day-to-day function and survival, as well as how these should be taken into account when considering opioid drug regimens.
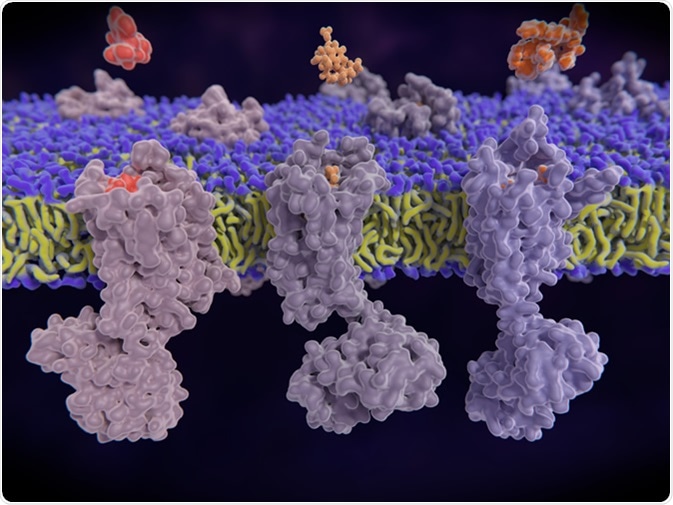
The system comprises three families of opioid peptides – neurotransmitters that are derived from proteolytic cleavage of more abundant precursor proteins – and three families of receptors. The three families of peptides are β-endorphin (derived from the precursor proopiomelanocortin); leucine (Leu)- and methionine (Met)-enkephalins (derived from preproenkephalin); and dynorphins, including dynorphins A and B and neoendorphins (all derived from preprodynorphin).
These opioid peptides bind to their G-protein-coupled receptors – the µ-opioid receptors, the δ-opioid receptors, the κ-opioid receptors, and the non-opioid receptor nociceptin (NOC – previously called opioid receptor-like 1 receptors).
β-endorphin mainly binds to µ-opioid receptors; the Met- and Leu-enkephalins primarily bind to δ-opioid receptors and µ-opioid receptors, while dynorphin and related peptides mainly bind to κ-opioid receptors. Nociceptin/orphanin FQ is the peptide that binds to NOC.
What roles does the system play?
The endogenous opioids and their receptors are widely distributed throughout the central and peripheral nervous systems, particularly the parts of these systems that regulate pain, emotion, reward, stress responses, motivation, drug addiction, and autonomic control. The differential expression and location of the various receptor subtypes across different neurons account for the wide range of opioid-related behaviors.
The activation of µ-opioid receptors is mainly known for playing a role in pain relief. Still, research has also indicated it may be involved in behaviors related to survival, such as appetite and reproduction. The activity of µ-opioid receptors is also known to play a critical role in responses to social stimuli by modulating responses to social rejection or social acceptance, for example.
Activation of the δ-opioid receptors and κ-opioid receptors is also known to be involved in pain modulation. Also, studies have shown that NOP activation is involved in pain mechanisms and several behaviors related to psychological stress.
Alterations in the endogenous opioid system are suspected to be involved in Parkinson's disease, seizures, neuroprotective mechanisms, and depression.
Endogenous opioids and addiction
Since the discovery of the endogenous opioid system, researchers have established its role in addiction. Drug addiction is characterized by adaptive alterations in the brain's reward circuits. Endogenous opioids and their receptors modulate dopaminergic activity and the cortisol response to stress, both of which are involved in the reward response to drugs and alcohol.
Research has shown that long-term use of exogenous opiates causes a comparative deficiency in endogenous endorphins, which, in turn, leads to opiate seeking and contributes to the ongoing relapses seen in cases of addiction.
Further studies using animal models of addiction have demonstrated that the endogenous opioid system significantly influences the effects that addictive substances have. This has also been confirmed in human studies showing that variants in genes that encode opioid system components are associated with the risk of addiction to opiates, cocaine, and alcohol.
Research has shown that many drugs of abuse increase the concentration of dopamine in a brain region called the nucleus accumbens and it has been suggested that this may mediate the rewarding effects these substances have.
Post-operative pain and endogenous endorphins
Opioid drugs are commonly prescribed for post-operative pain, however, these medications adversely affect the body's natural pain management system by disrupting the function of µ-opioid receptors and inhibiting the release of β-endorphin.
In response to post-operative pain, the hypothalamus secretes corticotrophin-releasing hormone, which travels to the anterior pituitary gland, where it triggers the cleavage of proopiomelanocortin to generate β-endorphin. In the peripheral nervous system, the binding of β-endorphin to its µ-opioid receptor and its subsequent activation disinhibits the release of gamma-aminobutyric acid (GABA). This then inhibits the release of neurokinin 1, a protein involved in pain transmission. In the central nervous system, activation of the µ-opioid receptor by β-endorphin inhibits the release of GABA, which usually inhibits the release of dopamine. Consequently, there is an increase in the production of dopamine – the hormone associated with feelings of euphoria.
In post-operative pain, the effect of β-endorphin >is, therefore two-fold – it decreases pain and helps to induce a sense of pleasure, motivation, and well-being.
Since prescriptions opioids stop the production of β-endorphin and disrupt the function of µ-opioid receptors, their administration can prolong and intensify pain, as well as reduce feelings of well-being. This has prompted many doctors to seek alternative pain-relief regimens for post-operative patients, and researchers are investigating non-opioid approaches to pain control.
However, acute post-operative pain and pain related to traumatic injury can be quite serious, and physicians should not withhold pain relief using opioids when used in the short-term. Pharmacologic pain relief can be a useful adjunct when used to help patients return to normal functioning. Long-term use of opioids is not recommended when alternatives are available.
Sources
- Benarroch, E. Endogenous opioid systems. Current concepts and clinical correlations. Neurology 2012; 79 (8). DOI: https://doi.org/10.1212/WNL.0b013e3182662098. Available at: https://n.neurology.org/content/79/8/807
- Maldonado, R et al. The endogenous opioid system: A common substrate in drug addiction. Drug and Alcohol Dependence 2010; 108 (3): 183-194. https://doi.org/10.1016/j.drugalcdep.2009.10.011. Available at: www.sciencedirect.com/science/article/abs/pii/S0376871609004013
- Wand, GS et al. Chapter 4 – Endogenous Opiates, Addiction, and the Stress Response. Stress and Addiction. Biological and Psychological Mechanism 2007, Pages 85-104. https://doi.org/10.1016/B978-012370632-4/50007-3. Available at: www.sciencedirect.com/…/B9780123706324500073?via%3Dihub
- Zubieta, J et al. Endogenous opioid system dysregulation in depression: implications for new therapeutic approaches. Molecular Psychiatry 2019; 24: 576–587 (2019). doi:10.1038/s41380-018-0117-2. Available at: https://www.nature.com/articles/s41380-018-0117-2
- Kreek, MJ. Endogenous opioid system in addiction and addiction-related behaviors. Current Opinion in Behavioral Sciences 2017; 13: 196 -202. https://doi.org/10.1016/j.cobeha.2016.12.002 Available at: https://www.sciencedirect.com/science/article/pii/S2352154616302649
- Sullivan, MD and Ballantyne, JC. Discovery of endogenous opioid systems: what it has meant for the clinician's understanding of pain and its treatment. Pain 2017; 158(12): 2290-2300. doi: 10.1097/j.pain.0000000000001043 Available at: journals.lww.com/…/…_of_endogenous_opioid_systems___what_it.5.aspx
- Parsa, FD and Stephan, BC. Avoiding Opioids and Their Harmful Side Effects in the Post-operative Patient: Exogenous Opioids, Endogenous Endorphins, Wellness, Mood, and Their Relation to Post-operative Pain. Hawaii J Med Public Health 2016;75(3): 63–67. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4795331/
Last Updated: Feb 17, 2020

Written by
Sally Robertson
Sally has a Bachelor's Degree in Biomedical Sciences (B.Sc.). She is a specialist in reviewing and summarising the latest findings across all areas of medicine covered in major, high-impact, world-leading international medical journals, international press conferences and bulletins from governmental agencies and regulatory bodies. At News-Medical, Sally generates daily news features, life science articles and interview coverage.
Source: Read Full Article
