Adenoviruses are considered as excellent vectors for delivering target antigens to mammalian hosts because of their capability to induce both innate and adaptive immune system. Currently, adenovirus-based vaccines are used against a wide variety of pathogens, including Mycobacterium tuberculosis, human immunodeficiency virus (HIV), and Plasmodium falciparum.
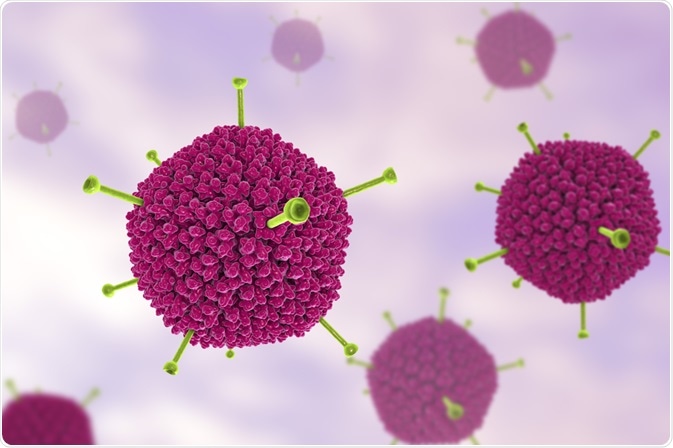
Image Credit: Kateryna Kon/Shutterstock.com
What are adenoviruses?
Adenoviruses are non-enveloped, double-stranded DNA viruses (genome size: 34-43 kb; virion size: 70-90 nm), first discovered in the human adenoid tissue in 1953 by Rowe and his colleagues. In humans, adenoviruses generally cause mild respiratory and gastrointestinal tract infections; however, adenovirus-induced infections can be life-threatening in immunocompromised people, or people with pre-existing respiratory or cardiac disorders.
These viruses are isolated from a wide variety of mammalian species, ranging from simians, chimpanzees to human beings. In humans, more than 50 adenovirus serotypes (no cross-neutralization by antibodies) have been identified, which are divided into 7 subgroups (A – G) based on red blood cell agglutination properties and sequence homology.
Adenoviruses express two types of genes: early genes and late genes. Early genes (E1A, E1B, E2, E3, and E4) are necessary for supporting viral replication inside host cells; whereas, late genes are required for host cell lysis, viral assembly, and virion release. Recombinant adenoviruses that are generated in the laboratory as vectors can be either replication-deficient or replication-competent.
Because the E1 gene is essential for viral replication, experimental depletion of the E1 gene generates adenoviruses that are capable of infecting the host cells but cannot grow in numbers because of defective replication. However, some specialized cells, such as HEK 293, can facilitate the replication of E1-deficient adenoviruses by providing E1 functions in trans.
What are the advantages of adenovirus-based vaccines?
There are several benefits of using adenoviral vectors for transferring viral antigens into host cells to trigger desired immune responses. For example, because of the relatively large-sized and well-characterized genome, adenoviruses are easy to manipulate genetically. Because adenoviruses cause mild infections in humans, as well as viral replication, can be inhibited by genetic modifications, adenovirus-based vaccines are mostly safe and come with very few side-effects.
These viruses are capable of infecting a wide range of dividing and nondividing cells because of broad tissue tropism. Other factors that make adenovirus-based vaccines more advantageous include higher thermostability, ability to grow to high titers, and easy application through systemic or respiratory mucosal routes.
Unlike other viral vectors, such as lentivirus and retrovirus, the risk of insertion mutagenesis is very less in the case of adenoviruses as they do not integrate the viral genome with the host genome.
Another major advantage of adenovirus-based vaccines is their ability to induce strong and sustained innate and adaptive immune responses. In particular, adenoviruses can induce both CD4+ T cell- and CD8+ T cell-mediated immune responses, which make them appropriate candidate vectors for developing vaccines against pathogens that are primarily eliminated by the cell-based immune system.
Neutralizing antibodies produced by adenoviral infections or adenovirus-based vaccines primarily target the viral capsid protein hexon; however, antibodies generated against the pentose base or fiber (other two capsid proteins) can also neutralize adenoviruses.
Moreover, adenoviruses express pathogen-associated molecular patterns (PAMPs) to induce the innate immune system. Binding of PAMPs with the host cell’s pathogen recognition receptor leads to the production of proinflammatory cytokines and maturation of antigen-presenting cells.
What are adenovirus-based vaccines?
To date, several adenovirus-based vaccines are in clinical and pre-clinical trials. Vaccines developed against HIV, Ebola virus, influenza virus, Mycobacterium tuberculosis, and Plasmodium falciparum are currently under human clinical trials. Moreover, there are vaccines under preclinical trials developed against rabies virus, dengue virus, and middle east respiratory syndrome coronavirus.
Adenovirus-based vaccines are prepared by inserting a transgene cassette into the adenoviral backbone through direct cloning or homologous recombination. The transgene cassette expresses the target antigen under the control of a strong promoter that is capable of maintaining robust and sustained expression of the transgene.

Image Credit: jaddingt/Shutterstock.com
Adenovirus-based tuberculosis vaccine
There is only one clinically approved tuberculosis vaccine namely Bacillus Calmette Guerin (BCG); however, this vaccine cannot protect against pulmonary tuberculosis. AdHu5 is the most commonly used human adenovirus serotype for the development of the tuberculosis vaccine.
The most widely studied adenovirus-based tuberculosis vaccine is E1/E2 depleted AdHu5 vector expressing immunodominant Mycobacterium tuberculosis antigen 85A, and the expression is controlled by the cytomegalovirus promoter.
One of the major drawbacks of this type of vaccine is that having preexisting immunity against AdHu5 can drastically reduce vaccine efficacy. This drawback can be subsided by using less prevalent serotypes, such as human adenovirus serotype 35. One such vaccine is rAd35-TBS, which is developed using the AdHu35 vector expressing three different antigens of Mycobacterium tuberculosis under the control of the cytomegalovirus promoter.
Adenovirus-based HIV vaccine
Trivalent AdHu5 vector expressing three HIV antigens, gag, pol, and nef, is the most widely studied HIV vaccine worldwide. However, this vaccine fails to reduce viral load clinically and increases the risk of HIV in AdHu5 seropositive males.
Another potential HIV vaccine candidate is the AdHu5 vector (replication-deficient) expressing simian immunodeficiency virus gag protein, and this vaccine has been shown to reduce viral load preclinically. Also, chimpanzee adenovirus (serotypes 3 and 63)-based vectors expressing gag, pol, and nef antigens have been shown promising results in the murine model.
Adenovirus-based influenza vaccine
Replication deficient AdHu5 vector expressing hemagglutinin antigen of avian influenza virus and a toll-like receptor 3 ligands has been found to induce antigen-specific immune responses in humans. Another novel approach is to use a chimpanzee adenovirus (AdC68)-based vector expressing artificial microRNAs to target matrix proteins or nucleoproteins of the influenza virus. Such vaccines have the potential to provide full protection from influenza infection by inhibiting viral replication.
Sources
- Tatsis N. 2004. Adenoviruses as vaccine vectors. Molecular Therapy. https://www.sciencedirect.com/science/article/pii/S1525001604013425
- Afkhami S. 2016. Methods and clinical development of adenovirus-vectored vaccines against mucosal pathogens. Methods and Clinical Development. https://www.sciencedirect.com/science/article/pii/S2329050116301735
- Zhang C. 2016. Adenoviral vector-based strategies against infectious disease and cancer. Human Vaccines and Immunotherapeutics. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4994731/
Last Updated: Sep 17, 2020

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article
