Point of care testing
NAAT
Lab-on-a-chip
Sequencing methods
Other techniques
Automation of laboratory testing
Sample collection
Pooled samples
Conclusions
References
Further reading
Infectious diseases (IDs) still take 14 million lives worldwide each year, making up a quarter of total deaths. This makes them a leading cause of mortality.
The management of IDs is dependent on accurate and rapid diagnosis. Beginning with Anton von Leuwenhoek’s first recording of animalcules, or bacteria, it progressed to the microbiological tests, including culture and staining techniques. However, these have advanced slowly compared to the stunning sophistication achieved in other diagnostic fields like biochemistry and radiology. Much effort has gone into reducing the time lag and the physical labor involved in this approach.

Image Credit: nito/Shutterstock
Not only are these techniques cumbersome and slow, but they require highly trained staff and carefully collected samples, usually body fluids. Both the accuracy, in terms of sensitivity, specificity, and the negative and positive predictive value, and the benefit of these tests, in terms of patient health, are equally desirable for any laboratory technology.
It is worth noting that researchers have come up with ASSURED characteristics that delineate the ideal diagnostic test: Affordable, Sensitive, Specific, User-friendly, Rapid, Equipment-free, and Delivered to those in need.
Point of care testing
A major advance in this field has been the entrance of rapid point of care tests (POCTs). These comprise rapid diagnostic tests (RDTs) based on direct microscopy or antibody-based antigen recognition methods. These include agglutination, enzyme-linked immunosorbent assays, optical immunoassays, and lateral flow assays (LFAs) based on immunochromatography.
Such tests are currently available for Chlamydia, many diarrheal agents, respiratory tract pathogens, reproductive tract disease, Treponema, Trichomonas, and some fungi. RDTs are often confirmed by additional tests, either based on antigens or nucleic acid testing.
Direct microscopy in clinical samples depends on observation of the pathogen in the tissues, often using histological stains or complemented by immunological or nucleic acid-targeting stains. Fluorescent labeling may add to the utility of the latter.
Antibody-based methods depend on the passage of the patient's antigen-containing sample through a matrix within which antibodies are bound. The resulting binding yields a colorimetric, fluorescent, or similarly easily interpreted readout.
Aptamers binding certain microbial components with high affinity may be substituted for the more heat-fragile antibodies, thus making RDTs more tolerant of tropical climates in future versions. Signal enhancement is another area that requires improvement to boost the sensitivity of these tests at low analyte concentrations. Antibody arrays on one platform are also being considered to enable screening for or diagnosis of any of multiple IDs using a single test.
The large scale of COVID-19 testing has allowed the comprehensive evaluation of these tests compared with the gold standard, whether the polymerase chain reaction or other benchmark test. The stability, manufacturing strength, operational standards, and potential for technical errors due to the lack of skill of those administering the test cannot match the standards of formal laboratory testing. However, they may be very useful when more sophisticated tests are ruled out for reasons of cost, availability, or technical factors.
For instance, these POCTs are often used to repeatedly screen asymptomatic workers or school children at regular intervals.
A second type of POCT is based on molecular diagnosis, with the results being available in minutes rather than hours. Its validity remains to be established by ongoing research. Two new platforms based on mass spectrometry are matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) and polymerase chain reaction (PCR)-electrospray ionization (ESI) mass spectrometry.
MALDI-TOF targets the detection of microbial cultures in conditions like urinary sepsis, where culture is both time-consuming and often inaccurate. Based on the detection of ribosomal proteins by mass spectrometry (MS), it is highly regarded for its speed, low cost, and simplicity of operation. It is in use in many European laboratories, though work continues to improve its discrimination of several species.
Some scientists claim that “MALDI is rapidly becoming the method of choice for identifying anaerobic bacteria.” It is often supplemented by urine flow cytometry. While it is mostly used to identify specimens in culture, it may be improved for use on primary samples.
PCR-ESI MS can be developed to diagnose most pathogens with speed and accuracy.

Image Credit: MilanMarkovic78/Shutterstock
NAAT
Various nucleic acid-based probes and nucleic acid amplification tests (NAATs), such as the polymerase chain reaction (PCR), have been around for over three decades. These are often considered to represent the future of microbiology due to their relatively rapid but high-quality results.
NAATs came to the forefront with the advance of the coronavirus disease 2019 (COVID-19), and many automated devices for high-throughput testing were introduced during the pandemic. These addressed issues such as a long turnaround time (TAT) and the handling time.
Several steps have been accomplished to reduce the TAT while increasing the throughput. Non-PCR technologies, including a range of Transcription Mediated Amplification (TMA)-based tests, isothermal amplification tests like loop-mediated isothermal amplification (LAMP), and Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas-based tests, along with many others, have entered the arena.
Isothermal amplification technologies dispense with the need for a thermocycler but are supposed to amplify nucleic acid at least as efficiently as PCR, making them cheaper and less sophisticated.
LAMP can cover a larger array of targets than conventional PCR and generate more amplified nucleic acid. However, the enzymes used are often inhibited by other substances in the human samples, while the primers are complex. Multiplexed assays are still uncommon with this platform.
CRISPR is among the biggest breakthroughs of the last couple of decades and can be combined with other technologies to detect nucleic acid at very low levels and with great rapidity. Some examples are Specific High-Sensitivity Enzymatic Reporter UnLOCKing (SHERLOCK) and DNA Endonuclease-Targeted CRISPR Trans Reporter (DETECTR), as well as RT-LAMP-CRISPR combinations.
Other advances in NAAT technology include the ability to reduce the number of samples per batch, down from 96 to as low as one, simply by using separate extraction and amplification modules. This segregation of the various steps allows the laboratory to load new samples, whether small batches or single samples, before the previous batch has been completely tested. The outcome has been the ability to perform a thousand or more tests per day per instrument.
Lab-on-a-chip
Microfluidics has enabled the development of lab-on-a-chip devices, integrating molecular amplification, molecular hybridization, and sophisticated optical or electrochemical detection to identify disease biomarkers in a single, inexpensive system, compatible with a hand-held or portable device.
Cepheid and Veredus have developed prototypical platforms that are currently being used. These still require an energy input, temperature- and storage-stable reagents, and easily interpreted readouts, which may limit their applicability in resource-constrained settings. Simplified versions may be necessary for this situation.
Simultaneously, more automation has been introduced, reducing hands-on time and test complexity. Built-in bar codes allow the specimen and reagent to be tracked while data is entered automatically via computer-instrument interfaces in the laboratory.
Sequencing methods
Other steps include sequencing of ribosomal ribonucleic acid (rRNA), such as the 16S rRNA gene in bacteria, and the 28S rRNA regions and the intergenic transcribed spacer (ITS) in fungi.
Next-generation sequencing (NGS) is a high-throughput platform in which sequence reads are generated at a very large scale in a parallel process. It has also revolutionized the sequencing of pathogens, both for individual infections and microbiome analysis. This helps, for instance, to deal with drug resistance or to track potential outbreaks.
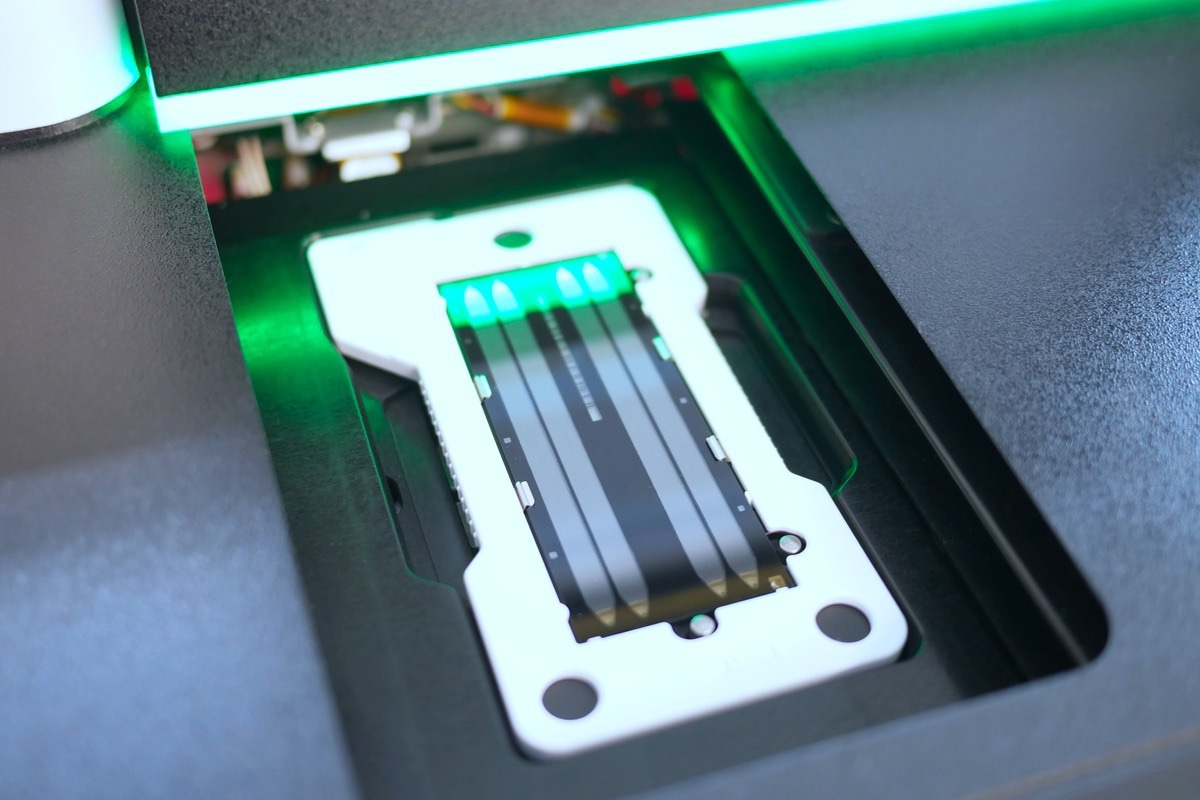
Image Credit: Elpisterra/Shutterstock.com
Other techniques
RNA hybridization and digital counting is a tool being developed to detect very small amounts of nucleic acid. Another completely automated platform uses RNA amplification and hybridization coupled with superparamagnetic particles to detect specific amplicons.
Nanoparticle-based tests, such as those from Nanosphere, that have gained FDA approval, are becoming popular but require sophisticated technology to deliver purified target molecules at adequate concentrations to the sensor area of microfluidics or nanosensor devices.
Opto-mechanical detection platforms may use aptamer or nucleic acid probes, antigens, or antibodies to recognize particles, as with surface plasmon resonance (SPR) biosensors or Young interferometry. This will avoid the need for microbial or component extraction.
Automation of laboratory testing
A third front where improvement is required is the introduction of automation to replace direct handling by trained laboratory and medical staff for very complex assays. The advantages are many, including higher reproducibility, a lower chance of error, independence from workforce shortages, higher throughput, and even the conservation of reagents and specimens with the use of microfluidics, in some cases.
These will not be completely human-free since trained staff must run the whole workflow, keeping reagent stocks high, overseeing the results, and intervening as required by the platform. Much effort will be needed to ensure that these instrument systems perform smoothly and, as required, to generate results comparable with the current gold standard.
Sample collection
Sample collection has also become an area of increased research in the search for non-invasive and at-home sample collection methods. More work is required, on a larger scale, with careful documentation, to compare the efficiency of various sample types in the diagnosis of rapidly spreading pathogens. While this may be very useful in blocking the spread of infection, by allowing for the earlier identification of cases, care must be taken to collect the specimen accurately.
Pooled samples
Using pooled samples is a strategy that both speeds up results and conserves reagents and specimens. If a pool of samples is negative on testing, all the individual samples are declared negative, while positive results necessitate the individual testing of each of the samples in the pool. It is most useful during situations when the prevalence of infection is low, and the supply of reagents is limited.
The limitations of this approach lie mainly in the need to pool samples with a low margin of error and with limited human handling of specimens.
Conclusions
As rapid diagnosis and initiation of treatment become recognized as essential components of ID management,
RDTs performed by minimally trained medical staff may enhance the cost-effectiveness of screening, and translate into better management of infections. In these conditions, global health improvement will permit the introduction of more elaborate diagnostic technologies in reference-level facilities, in an effort to develop a technical and technological capacity for national healthcare systems.”
References
- Bissonnette, L. et al. (2010). Diagnosing Infections—Current and Anticipated Technologies for Point-Of-Care Diagnostics and Home-Based Testing. Clinical Microbiology and Infection. https://doi.org/10.1111/j.1469-0691.2010.03282.x. https://www.sciencedirect.com/science/article/pii/S1198743X14641938.
- Peaper, D. R. et al. (2022). Advances in Molecular Infectious Diseases Testing in The Time of COVID-19. Clinical Biochemistry. https://doi.org/10.1016%2Fj.clinbiochem.2022.02.005. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8843810/.
- Hu, Z. D. et al. (2020). Laboratory Diagnosis Of Infectious Diseases: A Call For More Rapid And Accurate Methods. Annals of Translational Medicine. doi: 10.21037/atm-2020-id-13. https://atm.amegroups.com/article/view/42416/html.
- Pecora, N. et al. (2018). New Technologies for the Diagnosis of Infection. Diagnostic Pathology of Infectious Disease. https://doi.org/10.1016%2FB978-0-323-44585-6.00006-0. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7152403/.
- Srivastava, S. et al. (2018). Developments in the Diagnostic Techniques of Infectious Diseases: Rural and Urban Prospective. Advances in Infectious Disease. https://doi.org/10.4236%2Faid.2018.83012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6124492/.
- Barac, A. et al. (2020). Editorial: Innovative Approaches in Diagnosis of Emerging/Re-emerging Infectious Diseases. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2020.619498. https://www.frontiersin.org/articles/10.3389/fmicb.2020.619498/full
Further Reading
- All Infectious Diseases Content
- Sex Differences in Infectious Diseases
- What is Reverse Zoonosis?
- How Does Travel Influence Spread of Disease?
- How to Prevent the Spread of Infectious Diseases
Last Updated: Jul 6, 2022

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
