Ask any neurologist: Parkinson’s disease is a brain disorder. The conspicuous symptoms of Parkinson’s disease—uncontrollable tremors, slowed down motions, and the feeling that one’s feet are stuck to the ground—all stem from the loss of neurons in a region of the brain that helps control movement.
But many researchers believe that the neurodegenerative disorder may get started far away from the brain—in the gut—and years before the first neurological signs appear.
New findings by Columbia researchers David Sulzer, Ph.D., and Dritan Agalliu, Ph.D., and two of their graduate students are adding to evidence backing this hypothesis—and showing that what triggers initial gastrointestinal changes in Parkinson’s could be a misdirected immune attack.
“If this is the beginning of Parkinson’s in many people, videos do urso bernard we could potentially identify who has the disease before it ever reaches the brain and hopefully stop it in its tracks,” Sulzer says. The new findings were published Aug. 18 in Neuron.
Autoimmunity and the gut
The gut-first theory of Parkinson’s, originally proposed 20 years ago, started to intrigue Sulzer after his own research pointed toward the role of an autoimmune response in Parkinson’s.
In Parkinson’s, a protein called alpha-synuclein becomes misfolded, accumulates inside neurons, and slowly poisons the cells. Sulzer’s lab in collaboration with immunologists at the La Jolla Institute of Immunology has shown that small portions of the misfolded alpha-synuclein also can appear on the outside of neurons, which makes the neurons vulnerable to attack from the immune system. The immune attack could be doing more acute damage to the neurons than the internal deposits of alpha synuclein.
“The blood of Parkinson’s patients often contains immune cells that are primed to attack the neurons,” Sulzer says, “but it’s not clear where or when they are primed.”
The gut was an intriguing possibility because it contains the same neurons and because most Parkinson’s patients experience constipation years before brain symptoms emerge and the disease is diagnosed. To pursue this hypothesis, Sulzer teamed up with Agalliu, a neuroimmunologist with expertise in mouse models of another neurological disorder (multiple sclerosis) that has autoimmune features.

Immune response to alpha synuclein leads to gut symptoms
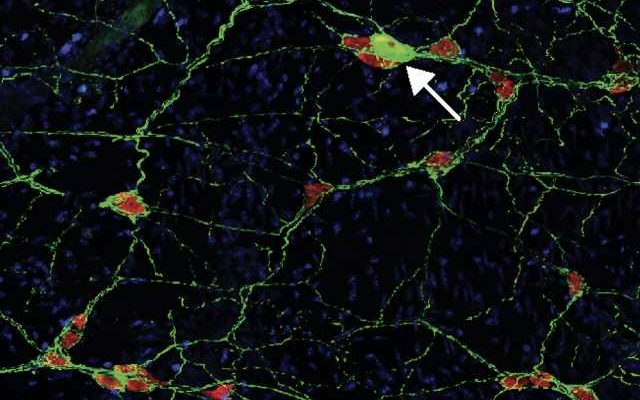
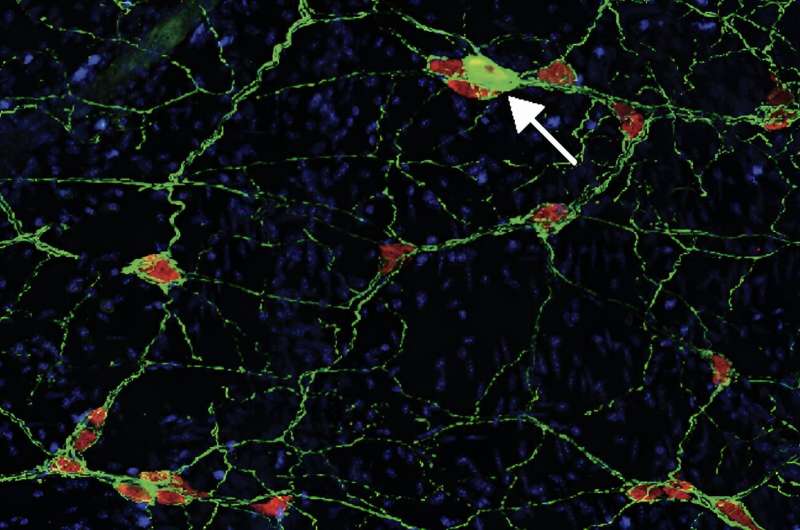
To find out if an immune reaction to alpha-synuclein can kick-start the disease and where, Francesca Garretti and Connor Monahan, grad students directed by Agalliu and Sulzer, first created a mouse capable of displaying pieces of misfolded alpha-synuclein on cell surfaces (natural mice do not have this ability). They then injected the mice with alpha-synuclein and monitored what happened in the brain and the gut.
The researchers did not see any signs resembling Parkinson’s disease in the brain, but they did see that an immune attack on neurons in the gut produced constipation and other gastrointestinal effects resembling those seen in most Parkinson’s patients years before they are diagnosed with the disease.
“This shows that an autoimmune reaction can lead to what appears to be the early stages of Parkinson’s and is strong support that Parkinson’s is in part an autoimmune disease,” Sulzer says.
The findings also raise the possibility that early detection—and then interruption—of an immune response in the gut could prevent a later attack on the brain’s neurons and stop Parkinson’s in its tracks.
Wanted: A mouse with Parkinson’s disease
Right now, though, it’s not clear how big a role the immune system plays in the Parkinson’s brain. The answer to that question may become clearer if the researchers find out why the brains of their mice did not develop any signs of Parkinson’s.
The team hypothesizes that the immune cells in their mouse model may not be reaching the brain because the animals are young and age has not yet weakened the blood-brain barrier sufficiently to let immune cells squeeze through. Opening the barrier or accelerating the aging process may lead to mice that develop gastrointestinal and brain symptoms.
“Our ultimate goal is to develop a model of Parkinson’s disease in mice that recreates the human disease process, which doesn’t exist right now,” Sulzer says. “That will be critical in answering questions about the disease that we can’t explore in people and eventually developing better therapies.”
More information:
Francesca Garretti et al, Interaction of an α-synuclein epitope with HLA-DRB1∗15:01 triggers enteric features in mice reminiscent of prodromal Parkinson’s disease, Neuron (2023). DOI: 10.1016/j.neuron.2023.07.015
Journal information:
Neuron
Source: Read Full Article