In a new study, researchers from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, identified factors that were associated with primary care practices successfully improving the quality of cardiovascular preventive care without increasing burnout among clinicians and staff.
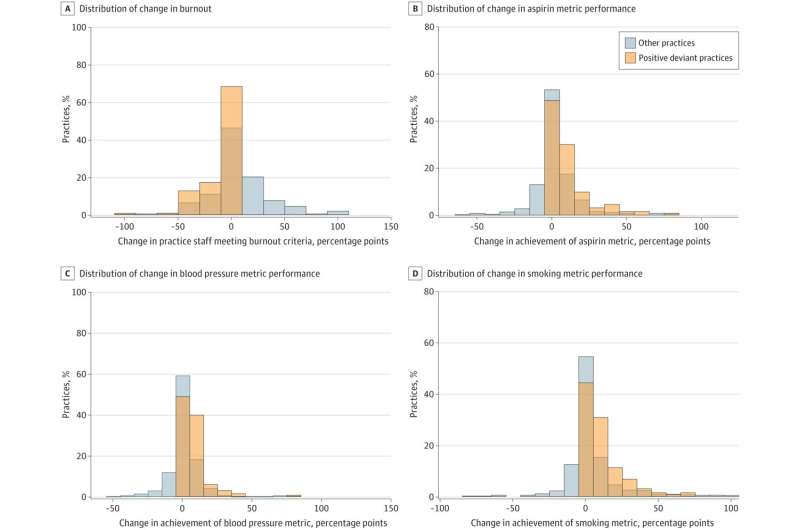
They analyzed 727 small and medium sized primary care practices for improvements in aspirin prescribing, blood pressure control, and smoking cessation counseling as proxies for quality of preventive care. They assessed which of the practices with improvements in quality had decreases or no increase in the percentage of staff reporting burnout over the study period.
They found that across practices of varying size, geography, and composition, 18.3 percent met the criteria to be considered quality and well-being promoting practices. Among all the factors evaluated, they found clinician-owned practices had statistically significant greater odds of improving quality without increasing burnout among clinicians and staff compared to hospitals owned by a health system. Future studies are needed to evaluate more detailed cultural factors that may contribute to these outcomes.
“This study is unique in identifying factors associated with improving both quality of patient care and staff experience, timolol maleate depression ” said first author Lisa S. Rotenstein, MD, MBA, and primary care physician at Brigham. “Our findings add to a growing body of research suggesting positive satisfaction, engagement and utilization outcomes among clinician-owned practices.”
The paper is published in the journal JAMA Health Forum.
More information:
Lisa S. Rotenstein et al, Association of Clinician Practice Ownership With Ability of Primary Care Practices to Improve Quality Without Increasing Burnout, JAMA Health Forum (2023). DOI: 10.1001/jamahealthforum.2023.0299
Journal information:
JAMA Health Forum
Source: Read Full Article