<img class="aligncenter" src="https://scx1.b-cdn.net/csz/news/800a/2023/comparison-with-canada.jpg"
alt="Comparison with Canada highlights poor access to US methadone treatment"
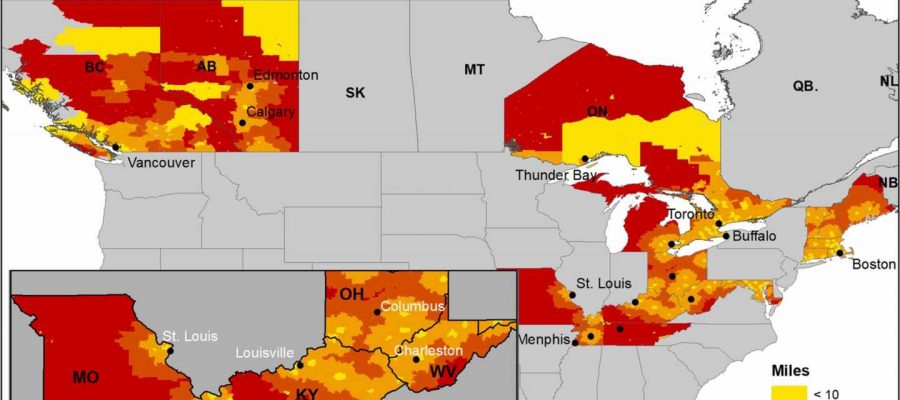
title="Driving distance to methadone clinic accepting new patients within 48 h among census tracts and areas fourteen US and three Canadian jurisdictions 2020. NOTES [In order to compare income within states and provinces, we normalized the income within each state (Connecticut, District of Columbia, Kentucky, Maine, Massachusetts, Maryland, Michigan, Missouri, New Hampshire, soma penalty group texas Ohio, Rhode Island, Tennessee, Vermont, and West Virginia) or province (Alberta, Ontario, and British Columbia). Credit: Drug and Alcohol Dependence (2023). DOI: 10.1016/j.drugalcdep.2023.109801″ width=”800″ height=”530″>
People living in the United States must travel significantly farther to access methadone treatment for opioid addiction than Canadians, suggests a new study led by Washington State University researchers.
Published in the journal Drug and Alcohol Dependence, the researchers’ analysis showed that the average driving distance to the closest methadone clinic accepting new patients was more than three times greater in the U.S. compared to Canada. When limiting their analysis to clinics that could provide treatment within 48 hours the difference was even larger, with those in the U.S. having to travel more than five times farther than their neighbors north of the border.
“Our research suggests that the U.S. could benefit from adopting Canada’s more flexible regulatory approach to methadone treatment, which is associated with greater availability of timely treatment, especially in rural areas,” said lead study author Ofer Amram, an assistant professor in the WSU Elson S. Floyd College of Medicine.
Amram explained that those seeking methadone treatment in the U.S. must start their treatment and receive their daily dose of methadone at federally approved treatment clinics, which in rural parts of the country can be far and few between. In Canada, methadone is prescribed not only in more widely available treatment clinics but also through trained primary care providers. Once treatment has started, Canadian patients can pick up their daily methadone dose at a local pharmacy.
The WSU team, who worked with researchers at Yale University and Simon Fraser University in Canada on the study, analyzed data collected from 563 methadone clinics accepting Medicaid or provincial insurance. These clinics were located in 14 U.S. states and three Canadian provinces that had the highest opioid overdose rates within each country.
The researchers calculated the driving distance from 17,611 census tracts within those states and provinces to the nearest clinic accepting new patients. After adjusting for differences in population density and demographics, they found that U.S. census tracts were an average of 11.6 miles farther from the closest methadone clinic accepting new patients. For clinics that could take in new patients within 48 hours, the distance gap was even wider at an average of 25.1 miles farther in the U.S. than in Canada.
For rural areas of the U.S. where the population is more spread out, the researchers found that access to a clinic providing treatment within 48 hours required lengthy drives of as many of 138 miles. Amram said this was especially true for rural areas of Tennessee, Kentucky and Missouri.
Amram noted that their comparison only looked at methadone treatment clinics—Canadian primary care providers prescribing methadone were not included.
“What that tells us is that the actual differences in treatment accessibility between the U.S. and Canada are even larger than our study suggests,” he said.
Data for the study were collected between mid-May and mid-June 2020, when both the U.S. and Canada had COVID-19 related policy exemptions in place that temporarily increased access to take-home methadone doses to facilitate social distancing. A previous study led by the WSU investigators showed that this increased flexibility in take-home dosing did not lead to worse treatment outcomes. The study was cited in recent guidance issued by the U.S. Substance Abuse and Mental Health Services Administration that extends methadone take-home flexibilities for one year past the end of the COVID-19 Public Health Emergency, which is set to expire on May 11.
“Our work adds to a growing body of evidence that suggests that better outcomes may be achieved by making these changes permanent along with expanding treatment to additional outpatient settings such as primary care clinics and community pharmacies,” Amram said. “Given the magnitude of the opioid overdose crisis, it’s important that we consider all the tools available to us to reduce barriers to treatment.”
More information:
Ofer Amram et al, Availability of timely methadone treatment in the United States and Canada during COVID-19: A census tract-level analysis, Drug and Alcohol Dependence (2023). DOI: 10.1016/j.drugalcdep.2023.109801
Journal information:
Drug and Alcohol Dependence
Source: Read Full Article