Researchers led by Professor Carolyn King of the University of Basel have developed a method to study the specialization of T cells in the context of infections. In the journal eLife, they report the different directions this specialization takes, depending on whether it happens in the context of an acute viral infection such as influenza or a chronic one such as HIV infection or malaria, which can no longer be overcome by the body.
The study focused on so-called T-helper cells. When such a cell is activated by a viral infection, it can specialize in one of two ways: into a Th1 cell, which drives a more inflammation-heavy T killer cell response, or into a T follicular helper (Tfh) cell, which primarily supports antibody production. The balance between Th1 and Tfh cells therefore has important implications for how inflammatory the body’s immune response is.
Degree of activation sets the tone
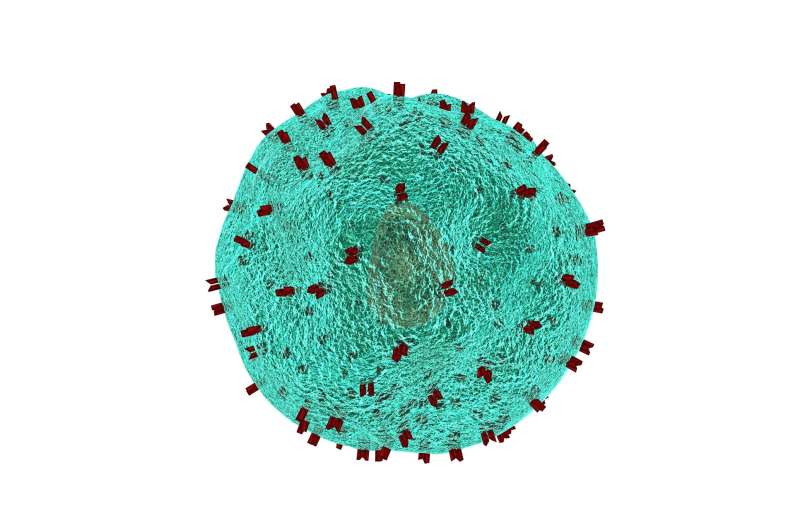
However, there are still gaps in our knowledge of how exactly a T helper cell decides which path to take when specializing. One factor that may play an important role is how strongly the T helper cell is activated—or, synthroid and infertility more precisely, its T cell receptor. The T-cell receptor is a kind of molecular sensor on the surface of the cell that more or less matches a part of the pathogen. The better they match, the more the receptor is activated.
Until now, however, it has not been possible to study the role of T-cell receptor signaling strength in the context of viral infections because researchers lacked a suitable experimental model. King and her team have now been able to develop one in collaboration with the research group of Professor Daniel Pinschewer, like King at the Department of Biomedicine.
Opposing effects in acute and chronic infection
The results of their analysis surprised the researchers: T-cell receptor activation does play a role, but an opposing one, depending on whether the infection was acute or chronic. Strong activation led to more inflammatory Th1 cells in acute viral infection. However, in chronic infection, strong activation produced more non-inflammatory Tfh cells.
“The reason behind this could be an evolutionary adaptation of nature to protect its own body,” explains Dr. Marco Künzli, first author of the study. “If too many inflammatory Th1 cells are produced for too long during chronic infections, this would harm the body’s own organs in the long run.”
Stronger for longer
The experiments also yielded another interesting finding: Th1 cells that form as a result of weak activation could remain functional longer in chronic infection than if their specialization was triggered by strong activation of the receptor. This is relevant because Th1 cells “fatigue” over time in chronic infections.
“Our results add a piece to the puzzle of T cell exhaustion and might—as a first step—contribute to new approaches in treating chronic viral infections,” King summarizes the significance of the findings.
Measuring the fate of T cells
Source: Read Full Article
