<img class="aligncenter" src="https://scx1.b-cdn.net/csz/news/800a/2023/obesity-as-a-risk-fact.jpg"
alt="Obesity as a risk factor for colorectal cancer underestimated so far"
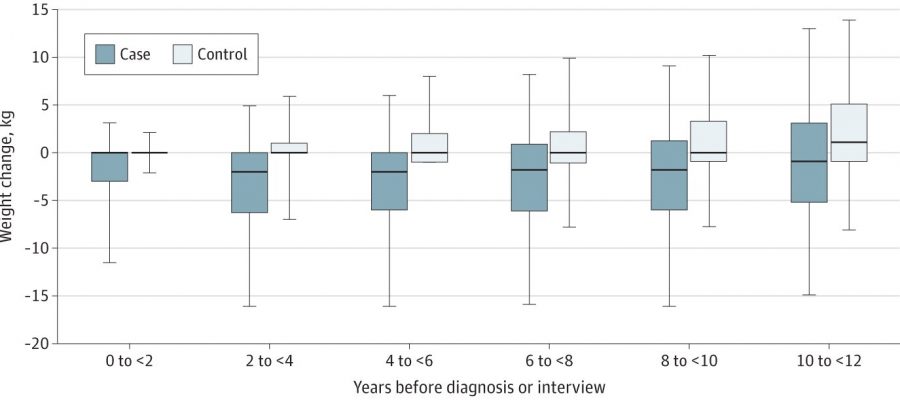
title="Weight Change Among Cases and Controls Within 12 Years Before Diagnosis/Interview Lower and upper hinges correspond to 25th and 75th quantile of weight changes, respectively; lower and upper whiskers correspond to 5th and 95th quantile, codeine overdose seizures respectively; outliers not shown. Credit: JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.9556″ width=”800″ height=”351″>
Obesity is a known risk factor for colorectal cancer. Scientists at the German Cancer Research Center (DKFZ) have now shown that this association has probably been significantly underestimated so far.
The reason: many people unintentionally lose weight in the years before a colorectal cancer diagnosis. If studies only consider body weight at the time of diagnosis, this obscures the actual relationship between obesity and colorectal cancer risk. In addition, the current study shows that unintentional weight loss may be an early indicator of colorectal cancer.
Obesity is a risk factor for a whole range of cancers. This association is particularly clear, for example, in the case of endometrial cancer, kidney cancer and also colorectal cancer. According to previous estimates, obese people have a risk of developing colorectal cancer that is about one-third higher than that of normal weight individuals.
“However, these studies have so far not taken into account that many affected people lose weight in the years before their colorectal cancer diagnosis,” says Hermann Brenner, epidemiologist and prevention expert at the German Cancer Research Center. “This has led to the risk contribution of obesity being significantly underestimated in many trials.”
To assess the magnitude of this bias, Brenner’s researchers evaluated data from the DACHS study. The nearly 12,000 study participants included in the current evaluation had provided information on their body weight at the time of diagnosis and had also reported their weight in the years preceding diagnosis (measured at 10-year intervals).
On the basis of body weight at the time of diagnosis, no indication of a relationship between body weight and colorectal cancer risk could be established. The picture was quite different, however, when the researchers looked at the participants’ earlier body weight: Here, a strong correlation between overweight and the probability of developing colorectal cancer was found, which was most pronounced 8 to 10 years before diagnosis.
Study participants who were highly overweight—referred to as obese—during this period were twice as likely as those of normal weight to develop colorectal cancer. “If we had only looked at weight at baseline, as has been done in many previous studies, we would have completely missed the link between obesity and increased risk of colorectal cancer,” says Marko Mandic, the study’s first author.
In their analyses, Brenner’s team was able to identify another trend: A striking number of the study participants affected by colorectal cancer had unintentionally lost weight before diagnosis. An unintentional weight loss of two kilos or more within two years prior to diagnosis (or study entry) occurred 7.5 times more frequently in cancer-affected individuals than in those in the control group.
“During this period, the cancer is already there, but not yet noticeable by symptoms. Doctors should therefore regularly ask their patients about unintentional weight loss,” Brenner says. “Unintentional weight loss could also be an early indication of other cancers or other diseases and should be carefully clarified.”
The study is published in the journal JAMA Network Open.
More information:
Marko Mandic et al, Association of Overweight, Obesity, and Recent Weight Loss With Colorectal Cancer Risk, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.9556
Journal information:
JAMA Network Open
Source: Read Full Article