A new study from Keio University, Japan, provides an evaluation of the effectiveness of relaxing public interactions following vaccination against the coronavirus disease 2019 (COVID-19). This study also presents data on the benefits following vaccination that may win over the vaccine-hesitant.
 Study: COVID-19 Vaccine Hesitancy And Vaccine Passports: Vaccination Or Restriction? Image Credit: Anishka Rozhkova / Shutterstock.com
Study: COVID-19 Vaccine Hesitancy And Vaccine Passports: Vaccination Or Restriction? Image Credit: Anishka Rozhkova / Shutterstock.com
Background
The COVID-19 pandemic has led to immense economic and health-related harm worldwide. Effective vaccines against COVID-19 have been developed at unprecedented speed in an effort to help achieve herd immunity against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pathogen.
Although the duration of protection and the efficacy of the different vaccines, especially in the face of newer variants of the virus, require long-term follow-up, their utility in helping to bolster immunity, at least in the immediate present, is undisputed by most. Most public health experts would agree that 70% or more of the population must be vaccinated to establish herd immunity.
The alternative might involve over 30 million deaths worldwide, by some estimates, before the virus burns out or becomes endemic.
Vaccine hesitancy
Vaccine hesitancy poses a significant challenge to achieving this goal. This phenomenon is heterogeneous across communities and regions but is clearly significantly hampering global vaccination efforts. While much research has gone into uncovering the components of this psychological state, it is difficult to find recommendations on how to overcome it.
It is important to understand why people accept vaccination. The World Health Organization (WHO) Sage Working Group on Vaccine Hesitancy developed the “three Cs vaccine hesitancy model.” In their model, confidence, complacency, and convenience are provided as the factors influencing this decision, all of which can be attributed to historical, cultural, systemic, socioeconomic, and personal factors.
Education, risk perception for the disease as well as the vaccines, and knowledge about these matters help shape an age-dependent and sex-dependent increase in acceptance among older people, and especially women, of vaccines. The ability to evaluate information about the severity of the disease and the benefits of vaccination may be key to this decision.
Individual factors also contribute to vaccine hesitancy, such as having an attitude that future benefits are less important than current costs. These factors also include negative perceptions due to mistrust and conspiracy beliefs, as well as being risk-averse.
However, external factors can also act on an unmotivated individual to incentivize a specific shift in decision-making, such as subsidies or regulations on personal freedom. Increasing the convenience and decreasing the costs of vaccination is also helpful.
One experiment suggests that providing attractive incentives in the form of public freedoms, to gather at recreational facilities or at homes, for instance, is an effective method of increasing vaccine acceptance. The new study, which is available on the medRxiv* preprint server, addresses these areas in terms of vaccination passports, which are being considered in many areas.
Though vaccine passports are still controversial in terms of their ethical concerns, their relevance can be considered if they are found to be likely to promote vaccine acceptance and thus help achieve population immunity.
Study findings
The researchers found a 30% vaccine hesitancy rate in a group of approximately 5,000 participants, at a time when almost 40% of the Japanese population had received one or more doses of the vaccine. This was reflected in the study group, thereby indicating that it was a representative sample.
87% of vaccine hesitancy concerns were related to the risks of vaccination, including side effects, with preference and mistrust of the vaccine also being commonly reported. The odds of these sentiments were higher for people between the ages of 25 and 44 years.
Older people between the ages of 55-74 years showed lower odds of vaccine hesitancy that were 17-67% lower by age. Females were almost 20% more likely to express hesitancy, while those caring for or living with older or sicker individuals had 16-44% higher odds of vaccine acceptance.
Frontline workers were less hesitant, though healthcare workers showed only 23% higher odds of vaccine acceptance compared to 71% for frontline essential workers. Hesitancy odds were 18% lower in those who were sicker.
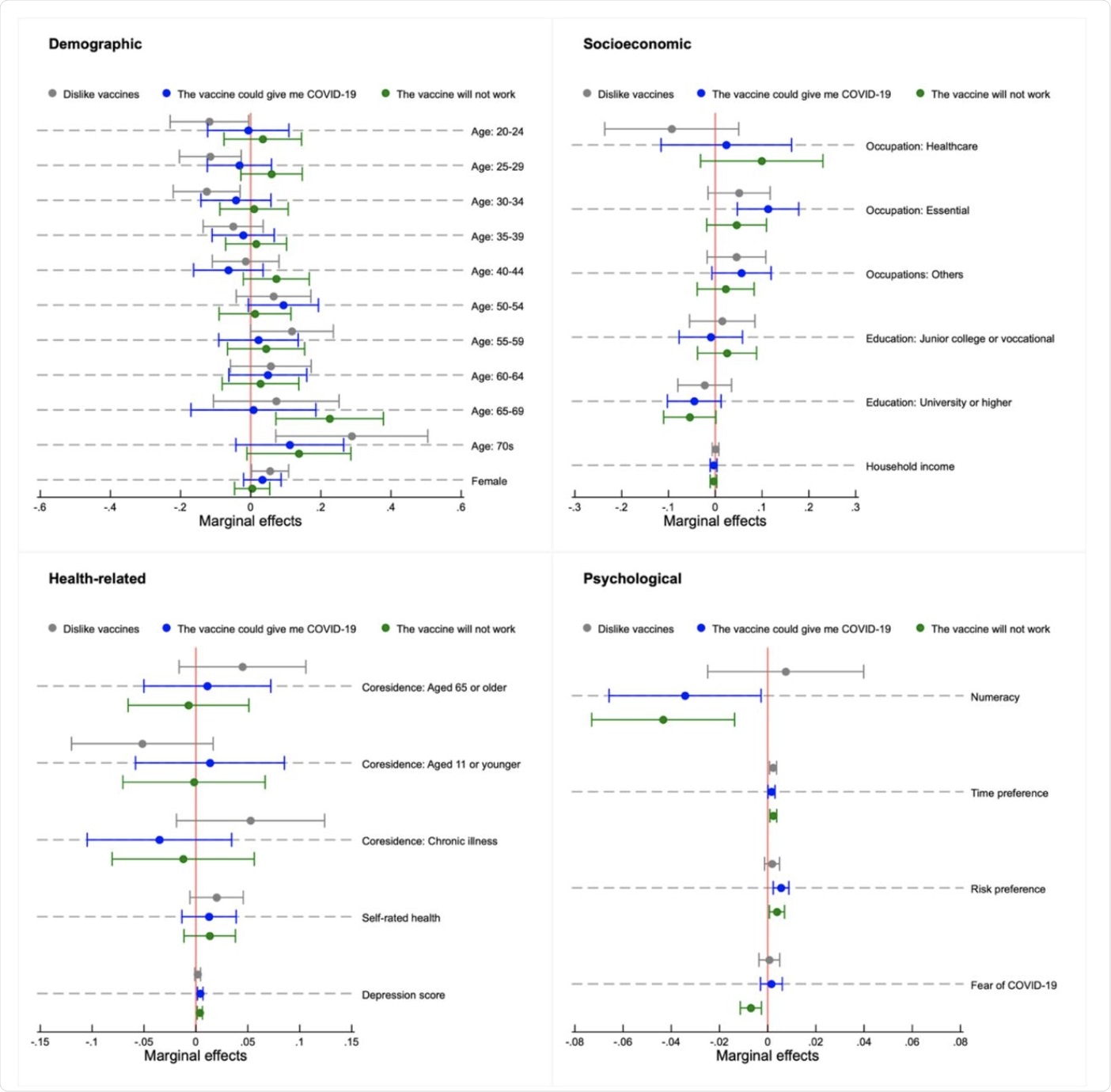 Determinants of reasons for vaccine hesitancy: Vaccine mistrust. Note: Analyses among individuals who were undecided and unwilling to vaccinate (n= 1,518); Markers represent marginal effects with error bars showing 95% confidence intervals estimated by robust standard errors; Adjusted for residential area with the population weight for each age group.
Determinants of reasons for vaccine hesitancy: Vaccine mistrust. Note: Analyses among individuals who were undecided and unwilling to vaccinate (n= 1,518); Markers represent marginal effects with error bars showing 95% confidence intervals estimated by robust standard errors; Adjusted for residential area with the population weight for each age group.
The role of public health restrictions was found to be a major contributor of vaccine hesitancy. To this end, almost 80% of participants said they would be vaccinated once all restrictions were removed; however, less than 60% indicated that they would accept the vaccines otherwise. Thus, the first situation was associated with a 4-10% increase in vaccine acceptance.
The most helpful relaxation in this respect was being able to cross prefecture lines, with 10% increase in acceptance with this step. Importantly, younger people followed the general trend, indicating that they would also be willing to be vaccinated if it allowed public health restrictions to be relaxed.
Implications
The current study is the first to explore this aspect of relaxing public health restrictions. The key findings are that vaccine hesitancy is closely related to socioeconomic, psychological, and health-associated factors, as well as age and sex. Younger people are significantly more likely to be hesitant.
Secondly, suspicion of the vaccines, related to a larger mistrust of the government, along with fears that the vaccines were unsafe or associated with significant side effects, was a major reason for vaccine hesitancy. This was again stronger in younger people.
Thirdly, letting people move about more freely, especially across prefecture borders, was key to vaccine acceptance in many cases, especially among younger people. This age group is at low risk for severe disease but is more likely to experience headache, fatigue, and other vaccine side effects. These factors could thus move them towards vaccine hesitancy.
In light of these findings, vaccine passports are likely to be useful in promoting vaccine acceptance, say the researchers. This could enable vaccinated people to move out of their homes, eat out, travel, gather with others in public, and participate in other important social interactions. This promise of normalcy may win many people tired of staying at home and keeping a social distance when outside.
Taken together, the researchers emphasize the need for clear communication on vaccine safety. To this end, public health messages should include the benefits of vaccination in non-health terms, as well as in more standard reference points such as reduced severity of symptoms and decreased risk of death from COVID-19 following vaccination.
“The continuous evaluations and careful consideration of the efficacy, duration of effectiveness, and side effects of the vaccine, as well as potential public health impacts and ethical issues of vaccine passports are indispensable.”
Vaccine passports should be limited in their duration, along with some type of viral containment measures, since vaccine immunity is not achieved in 100% of recipients.
“These types of passports must not be used to discriminate and eliminate those not vaccinating from society, allowing them to use alternative services, such as a certificate for a negative COVID-19 test result.”
Despite the limitations of this study, it offers key data on vaccine hesitancy among the Japanese population. It also provides a new way to enhance vaccine acceptance, along with educational campaigns to convey accurate information about the vaccine’s safety and side effects.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Okamoto, S., Kamimura, K., & Komamura, K. (2021). COVID-19 Vaccine Hesitancy And Vaccine Passports: Vaccination Or Restriction? medRxiv. doi:10.1101/2021.09.15.21263559. https://www.medrxiv.org/content/10.1101/2021.09.15.21263559v1.
Posted in: Men's Health News | Medical Research News | Miscellaneous News | Women's Health News | Disease/Infection News | Healthcare News
Tags: Coronavirus, Coronavirus Disease COVID-19, Education, Efficacy, Fatigue, Headache, Healthcare, immunity, Pandemic, Pathogen, Public Health, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
