Scientists have developed several pharmaceutical and non-pharmaceutical interventions to contain the current coronavirus disease 2019 (COVID-19) pandemic, which is caused by the rapid outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). For example, the rapid development of COVID-19 vaccines has been instrumental in the prevention of severe illness and deaths worldwide.
In Africa, owing to poor vaccination coverage, the intensity of severe infection and death due to SARS-CoV-2 infection remains high. Additionally, the emergence of new SARS-CoV-2 variants has reduced the efficacy of available vaccines and therapeutics, which are based on the spike protein of the original virus. The World Health Organization (WHO) has classified these SARS-CoV-2 variants as variants of concern (VOC) and variants of interest (VOI).
Study: Unsuppressed HIV infection impairs T cell responses to SARS-CoV-2 infection and abrogates T cell cross-recognition. Image Credit: Vecctor-3D / Shutterstock.com
HIV and COVID-19
The effect of COVID-19 in patients with human immunodeficiency virus (HIV) is not clear. In one study based on small sample size, researchers report that people living with HIV (PLWH) exhibited similar COVID-19 outcomes compared to healthy individuals.
However, a larger epidemiological study has contradicted the previous report and identified increased hospitalization and death rates due to COVID-19 among PLWH as compared to HIV-negative individuals.
One previous study revealed that prolonged shedding of high titers SARS-CoV-2 and the emergence of many mutations were found in individuals with advanced HIV and antiretroviral treatment (ART) failure. Scientists have stated that both B-cells and T-cells play important roles in providing protection against SARS-CoV-2 infection.
Interestingly, studies have shown that T-cell responses can offer protection even in the absence of humoral responses. This implies that in an individual with inherited B-cell deficiencies or hematological malignancies, T-cells will play an important role in their recovery from SARS-Cov-2 infection.
Previous reports have indicated that COVID-19 severity is related to a weak SARS-CoV-2-specific CD4⁺ T-cell polyfunctionality potential. Several studies have also shown that messenger ribonucleic acid (mRNA) vaccines can stimulate Th1 and Th2 CD4+ T-cell responses, which can be correlated with post-boost CD8+ T-cell responses and neutralizing antibodies. Thus, scientists have expressed the need for more insights regarding T-cell-mediated protection against SARS-CoV-2 infection.
About the study
In sub-Saharan Africa, the prevalence of HIV is high; thus, it is important to determine the effect of HIV in individuals diagnosed with COVID-19. Understanding the disease outcome in this patient population will help researchers and policymakers formulate effective strategies to protect them from SARS-CoV-2 infection.
A new study posted to the medRxiv* preprint server evaluates the impact of HIV infection on the quality and epitope specificity of SARS-CoV-2 T-cell responses during the first and second waves of COVID-19 in South Africa. In this study, scientists investigated the antigen-specific CD4+ and CD8+ T-cell responses in a cohort of SARS-CoV-2- infected individuals with and without HIV infection.
Herein, flow cytometry was used to estimate T-cell responses following peripheral blood mononuclear cell (PBMC) stimulation with SARS-CoV-2 peptide pools. The researchers also measured T-cell immunodominance hierarchies and determined the possibility of SARS-CoV-2 escape from T cell recognition through culture expansion.
Study findings
The first COVID-19 wave in South Africa was dominated by the wildtype D614G strain of SARS-CoV-2, whereas the second wave was dominated by the Beta variant. PBMCs were utilized to evaluate the effect of HIV infection on SARS-CoV-2 specific T-cell responses and determine T-cell cross-recognition.
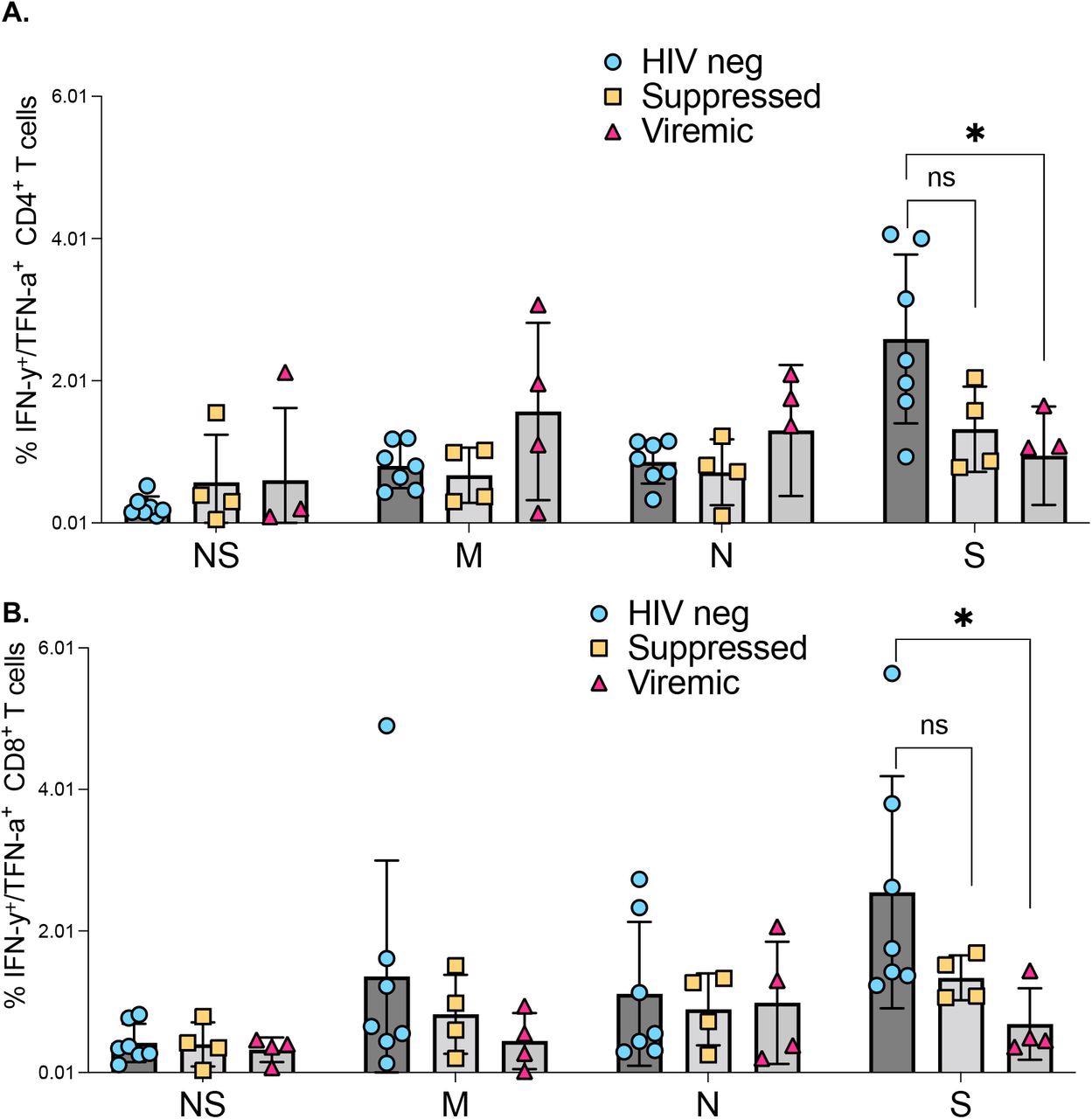
Comparison of SARS-CoV-2 protein targeting by T cell responses among HIV negatives, suppressed and viremic donors: The magnitude of (a) CD4+ T and (b) CD8+ T cell responses targeting SARS-CoV-2 proteins among study groups. P-values for differences among the groups are *<0.05; as determined by the Mann-Whitney U test. (GraphPad Prism version 9.3.0)
Impaired SARS-CoV-2 specific T-cell responses were identified in individuals with unsuppressed HIV infection. The researchers observed a low count of CD4+ T-cells, with hyperimmune activation, found to be related to reduced SARS-CoV-2 specific T-cell responses.
The scientists also determined spike mutations in the Beta variant, which caused abrogate recognition by memory T-cells raised against epitopes of the original SARS-CoV-2 strain. Likewise, immune responses against SARS-CoV-2 Beta variant epitopes poorly cross recognized corresponding original SARS-CoV-2 strain epitopes, thus demonstrating the ability of certain SARS-CoV-2 variants to escape T-cell recognition.
Individuals with unsuppressed HIV infection were found to exhibit poor responses to SARS-CoV-2 infection. Furthermore, HIV-induced immune defects such as low CD4+ T-cell counts, higher HIV plasma viral loads, and increased immune activation conferred reduced SARS-CoV-2 responses.
HIV-seronegative individuals exhibited robust CD4+ and CD8+ T-cell responses against the SARS-CoV-2 spike protein compared to the PLWH. Furthermore, reduced T-cell cross-recognition was observed between the two COVID-19 waves, which was more prominent in people with unsuppressed HIV infection.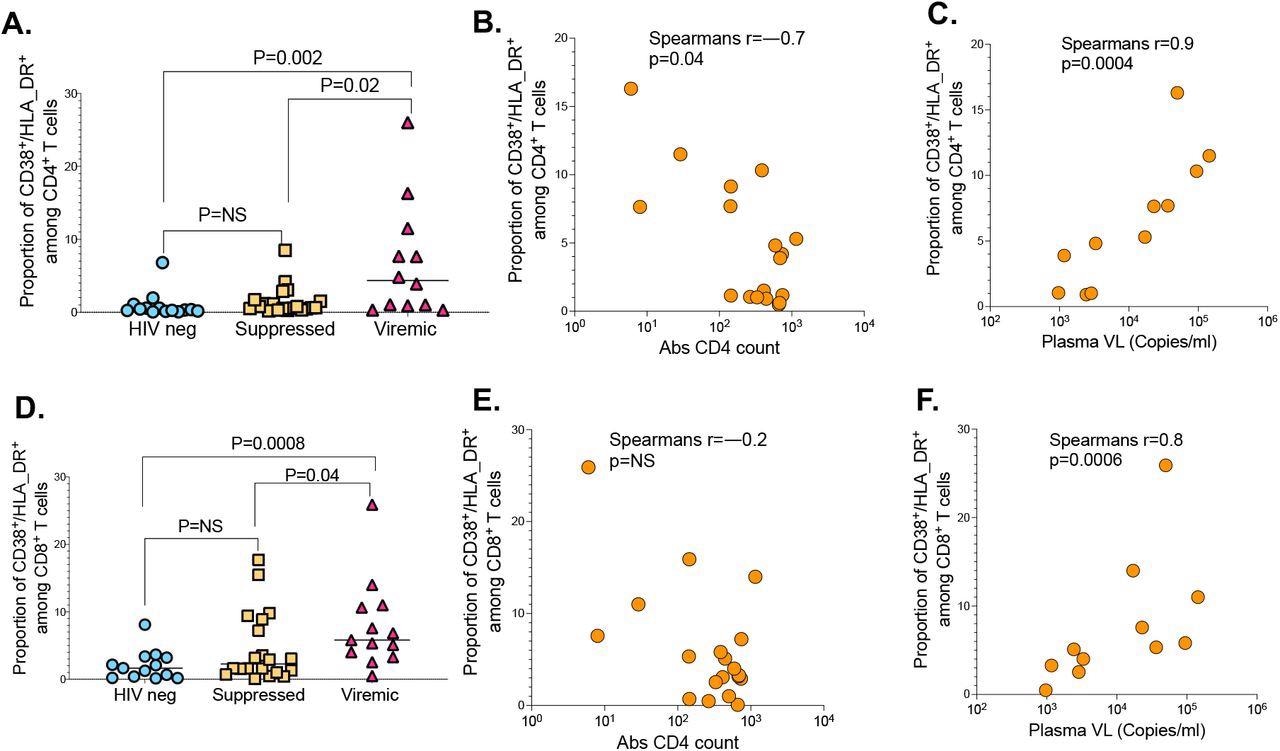
The impact of HIV markers of diseases progression on SARS-CoV-2 T cell immunity. (a) CD4+ T cell activation graphed based on the frequency of CD38/HLA-DR co-expressing cells. (b) Correlation between CD4+ T cell activation and absolute CD4 counts. (c) Correlation between CD4+ T cell activation and HIV plasma viral load. (d) CD8+ T cell activation measured by CD38/HLA-DR. (e) Correlation between CD8+ T cell activation and absolute CD4 counts. (f) Correlation between CD8+ T cell activation and HIV plasma viral load.
Conclusions
Unsuppressed HIV infection significantly impairs T-cell responses to SARS-CoV-2 infection and reduces T-cell cross-recognition. These findings explain the increased vulnerability of PLWH to severe COVID-19, as well as highlight their susceptibility to infection with emerging SARS-CoV-2 variants.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Nkosi, T., Chasara, C., Mbatha, A., et al. (2022) Unsuppressed HIV infection impairs T cell responses to SARS-CoV-2 infection and abrogates T cell cross-recognition. medRxiv. doi:10.1101/2022.04.05.22273453. https://www.medrxiv.org/content/10.1101/2022.04.05.22273453v1.
Posted in: Medical Research News | Disease/Infection News
Tags: Antibodies, Antigen, Antiretroviral, Blood, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytometry, Efficacy, Flow Cytometry, HIV, Immunodeficiency, Pandemic, Protein, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, T-Cell, Therapeutics, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
