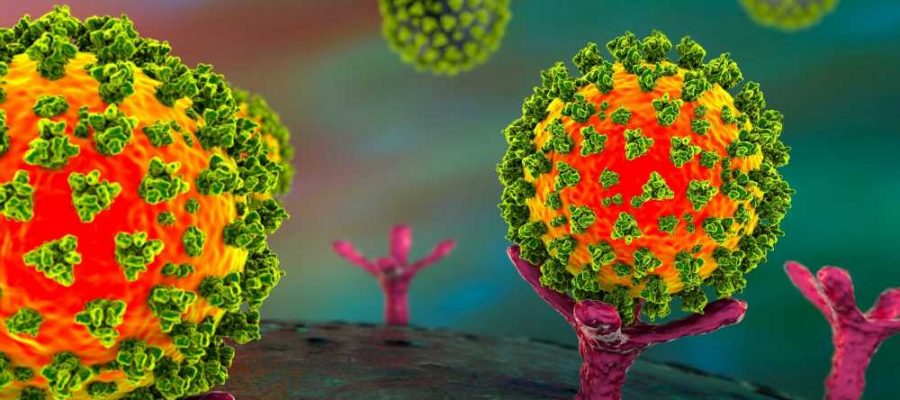
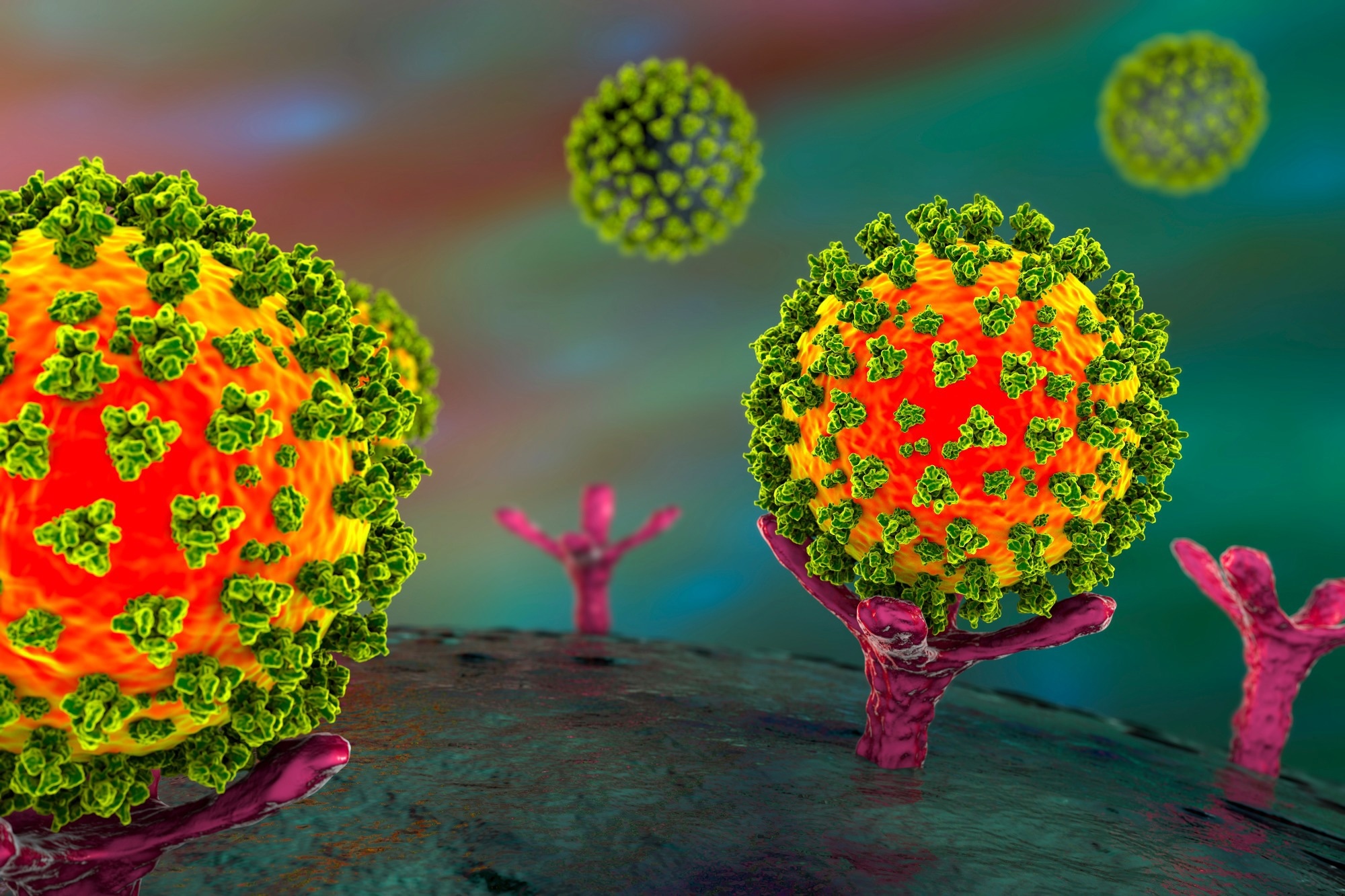
In a recent study posted to the bioRxiv* preprint server, researchers presented a microbody recombinant decoy protein with high affinity to angiotensin-converting enzyme 2 (ACE2) as an option for coronavirus disease 2019 (COVID-19) treatment.
Background
The continual emergence of increasingly immune-evasive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) VOCs (variants of concern) with multiple SARS-CoV-2 spike (S) protein mutations has challenged the efficacy of vaccines and monoclonal antibodies (mAbs) in the prevention and management of SARS-CoV-2 infections.
More effective prophylactic and therapeutic options are required to reduce the COVID-19 burden. The authors of the present study previously developed the pcACE2.mb receptor decoy protein against SARS-CoV-2 that potently neutralized the SARS-CoV-2 D614G strain and VOCs by binding to SARS-CoV-2 S, inhibiting the attachment of the S protein with human ACE2 (hACE2).
About the study
In the present study, researchers extended their previous analysis by modifying pcACE2.mb and testing its efficacy against SARS-CoV-2 VOCs in mice.
The pcACE2.mb potency was increased by incorporating the T27Y/L79T/N330Y mutations in the S protein that increase the S-ACE2 binding. In addition, the IgG1 CH3 domain of pcACE2.mb was truncated to increase the half-life. The decoy protein was transfected using ExpiCHO cells and purified by size exclusion and affinity types of chromatography. Pseudotyped lentivirus neutralization assays were performed to evaluate the anti-SARS-CoV-2 efficacy of pcACE2.mb.
The decoy binding affinity to SARS-CoV-2 S was evaluated based on virion binding assays and by evaluating the binding of sACE2 (soluble ACE2)-NLuc (nanoluciferase), ACE2.mb-NLuc, ACE2.1mb-NLuc decoy:nanoluciferase fusion proteins with SARS-CoV-2 S-expressing 293T cells. To assess the tissue localization of pcACE2.mb, proteins ACE2.1mb-NLuc, and sACE2-NLuc were intraperitoneally (i.p.) injected into mice, that were imaged for 3.0 days.
To evaluate the impact of the delivery route on ACE2.1mb distribution, the decoy protein was administered intraperitoneally, i.v. (intravenously) or i.n. (intranasally). To evaluate the decoy’s half-life in vivo, the activity of luciferase in pulmonary tissues and serum was assessed. Further, in vivo experiments were performed to evaluate the capability of the high-affinity ACE2.1mb decoy to prevent COVID-19, by administering the decoy by either route in hACE2-Tg mice with hACE2 knock-in.
Subsequently, mice were challenged with SARS-COV-2 USA-WA1/2020, and for comparative assessments, the animals were treated with REGN-CoV2, a mAb cocktail, following which pulmonary SARS-CoV-2 ribonucleic acid (RNA) was quantified at 3.0 days post-injection (dpi). BALB/c mice were used for evaluating the decoy’s efficacy against Omicron BA.1 and BA.2 sub-VOCs, in comparison to control mice treated with the LY-CoV1404 mAb or the REGN-COV2 cocktail.
Results
Immunology eBook
The recombinant decoy considerably reduced viral load in mice upon challenge with D614G, Omicron BA.1, and Omicron BA.2 and potently suppressed SARS-CoV-2 replication when administered post-infection, albeit with lower potency for the Omicron sub-VOCs. The decoy conferred broader protection against SARS-CoV-2 with similar potency compared to REGN-COV2 and greater protection than LY-CoV1404 mAbs. The ACE2.1mb decoy neutralized D614G with a 10.0-fold greater potency than sACE2, and the neutralization potency of the high-affinity ACE2.1mb was 5.0-fold higher.
In addition, the high-affinity microbody ACE2.1mb decoy was also highly potent against the Alpha VOC, Beta VOC, Gamma VOC, and Delta VOC but showed four-fold and six-fold lower binding to S proteins of Omicron BA.1 and Omicron BA.2, respectively. In mice injected intraperitoneally and intravenously, the decoy localized mainly to the serum, liver, and spleen, and of note, intravenous administration led to a 100-fold increase in decoy localization to pulmonary tosses. Intranasal administration localized the decoy to the trachea and lung.
The half-life of intravenously- or intranasally-injected decoy in serum was five days. In pulmonary tissues, the half-life of the decoy administered intravenously and intranasally was four days and eight days, respectively. The intraperitoneal, intravenous, and intranasal decoy administrations reduced the viral load by 108-fold and 15,700-fold, and 26,500-fold, respectively. Histopathological assessment of pulmonary tissues showed prominent immunological cell infiltration among untreated mice, which was almost absent in sACE2-treated mice and completely absent among ACE2.1mb-treated mice.
SARS-CoV-2 RNA was undetectable in the lungs over the course of the treatment. The intranasal and intravenous administration of 100 µg decoy suppressed SARS-CoV-2 proliferation to levels undetectable and 10 µg of the decoy suppressed SARS-CoV-2 proliferation by 12-fold. The intranasal administration showed slightly greater efficacy compared to intravenous administration at ten micrograms and 50 microgram doses.
The decoy reduced Omicron BA.1 viral load by 56.0-fold by intravenous administration and Omicron BA.2 by 100.0-fold by intranasal administration. Greater protection was observed in the case of decoy administration ≤2.0 days before COVID-19, and moderate protection was observed when administered at 3.0 dpi (200-fold reduction in viral load), with no protection at 5.0 dpi.
At 1.0 hours post-COVID-19, the intravenously- and intranasally-administered decoy reduced viral load by 1,100.0-fold and 27,500.0-fold, respectively. Similar findings were observed in the case of decoy administration after six hours of SARS-CoV-2 infection. However, after 12 hours of SARS-CoV-2 infection, the intravenously-injected decoy protein showed no significant effects. The intranasally-administered decoy reduced the viral load by 20-fold, consistently maintained up to 16 hours post-infection.
To conclude, based on the study findings, the high-affinity recombinant ACE2.1mb decoy protein could be a promising prophylactic and therapeutic option against SARS-CoV-2 VOCs and Omicron sub-VOCs.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Takuya Tada, Belinda M. Dcosta, Hao Zhou, and Nathaniel R. Landau. (2023). ACE2 Receptor Decoy is a Potent Prophylactic and Therapeutic for SARS-CoV-2. bioRxiv. doi: https://doi.org/10.1101/2022.12.31.522401 https://www.biorxiv.org/content/10.1101/2022.12.31.522401v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, binding affinity, Cell, Chromatography, Coronavirus, Coronavirus Disease COVID-19, covid-19, Efficacy, Enzyme, in vivo, Lentivirus, Liver, Luciferase, Lungs, Omicron, Proliferation, Protein, Receptor, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spleen, Syndrome

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article