Structural differences in lung airways between men and woman may be the cause of differences in chronic obstructive pulmonary disease (COPD) prevalence and outcomes between the sexes. According to a large, multicenter study published in the journal Radiology, researchers found that even among adults who have never smoked, or who have smoked less than 100 cigarettes in their lifetime, lung airways were smaller in women, which can lead to a higher risk for lung disease.
COPD refers to a group of diseases, such as emphysema and chronic bronchitis, that cause airflow blockage and breathing-related problems. More than 15 million Americans have COPD, according to the Centers for Disease Control and Prevention.
Overall, men have a higher rate of diagnosis and mortality, but with changes in smoking behavior and increasing urbanization, the prevalence of COPD in women is on the rise.
“The prevalence of COPD in women is fast approaching that seen in men, and airway disease may underlie some of the high COPD numbers in women that we are seeing,” said the study’s lead author, Surya P. Bhatt, M.D., M.S.P.H., associate professor of medicine, Division of Pulmonary, Allergy and Critical Care Medicine at the University of Alabama at Birmingham. “When airways narrow due to cigarette smoking, the impact on symptoms and survival is greater in women than in men.”
The assumption that women have smaller airways is based on comparisons of the trachea and main stem bronchi, but few studies have compared distal airways in normal individuals or accounted for differences in lung size.
For this study, researchers analyzed data from nearly 10,000 participants enrolled in Genetic Epidemiology of COPD (COPDGene), a prospective multicenter observational cohort study of current and former smokers, as well as never smokers, between the ages of 45 and 80 years, at 21 clinical centers across the United States. The researchers looked at data of never, current and former smokers enrolled in COPDGene from January 2008 to June 2011 and followed up longitudinally until November 2020.
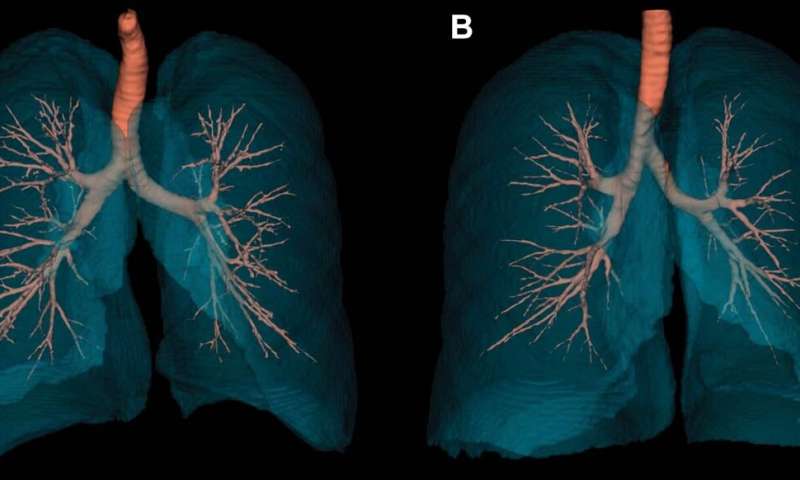
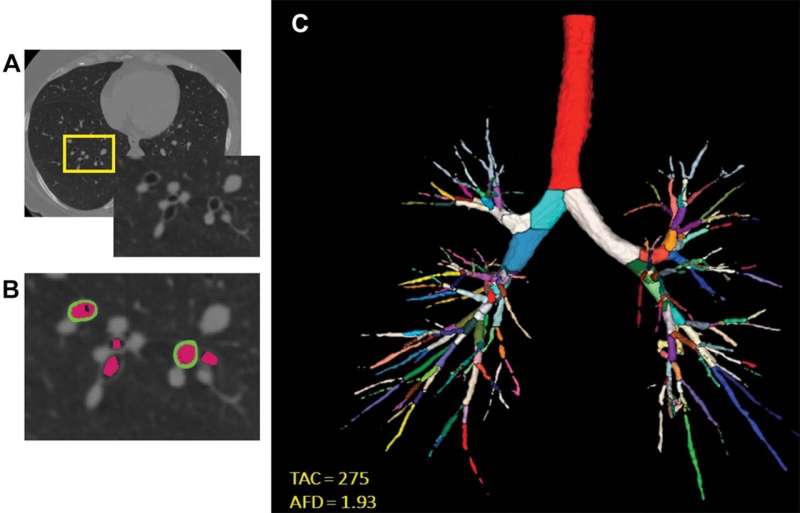
Airway disease on CT was quantified using seven metrics: airway wall thickness, wall area percent, Pi10 (square root of the wall thickness of a hypothetical airway with internal perimeter of 10 mm) for airway wall, lumen (airway passage in which air flows through) diameter, airway volume, total airway count and airway fractal dimension for airway lumen.
Each airway metric was calculated and adjusted for age, height, race, body mass index, pack-years of smoking, current smoking status and total lung capacity.
“The growth of airways and lungs in early life is generally more proportionate in women than in men,” Dr. Bhatt said.
In 420 never-smokers, CT scans revealed that men had thicker airway walls than women, whereas, after accounting for height and total lung capacity, airway lumen dimensions were lower in women than in men.
In 9,363 current and former smokers, men had greater wall thickness, whereas women had narrower segmental lumen diameter. A unit change in each of the airway metrics (higher wall or lower lumen measure) resulted in lower lung function, more dyspnea (shortness of breath), poorer respiratory-quality of life, lower six-minute walk distance and worse survival in women compared with men.
“The differences in airway dimensions even after adjusting for height and lung size, and the greater impact of changes in airway size on clinical outcomes in women, was remarkable in that women appear to have a lower reserve against developing airway disease and COPD,” Dr. Bhatt noted.
Source: Read Full Article
