Sepsis has a way of flying under the radar. Public awareness of the life-threatening disease is low, and official statistics are misleading. Now researchers are using special alarm systems and AI to increase detection.
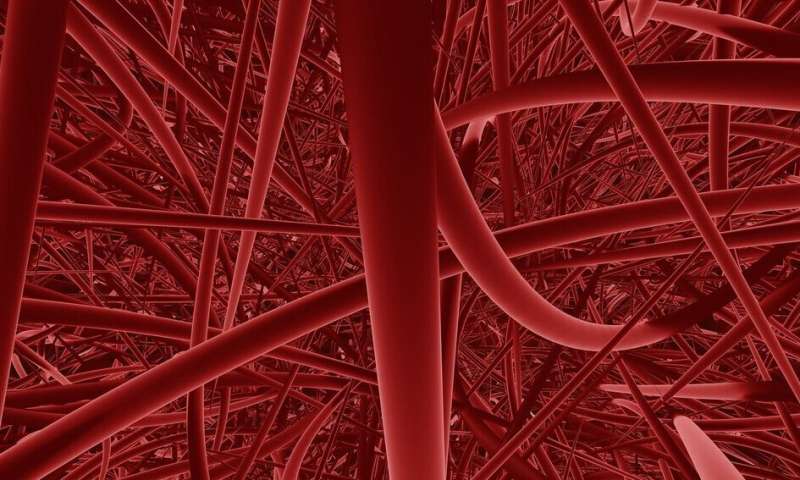
Do you know what sepsis is? Blood poisoning, you might say. And this is an older name for the disease, based on the belief that patients would always have bacteria in their blood. But in many cases, this is not the case. Instead, an infection somewhere in the body has put the immune system out of action. In that case, the infection itself is no longer the serious issue: the danger lies in the course of events that has been set in motion. Part of the chain may be that the immune system creates massive inflammation in the blood vessels, which are then impaired.
Awareness of the disease is low. Only 49% of the general public in Sweden think they know what sepsis is, according to a 2021 awareness survey conducted by Sepsisfonden. And there is also a great deal of uncertainty in Swedish sepsis statistics.
According to the National Board of Health and Welfare’s Cause of Death Register, more than 860 Swedes died from sepsis in 2021. But this is a highly misleading figure.
“This is one of many problems surrounding sepsis. Journalists and politicians get a false picture of how serious and common this disease when they rely on the National Board of Health and Welfare’s figures,” says infectious diseases doctor Kristoffer Strålin, researcher at the Department of Medicine at the Karolinska Institute in Huddinge.
The error occurs when doctors report to the National Board of Health and Welfare. Out of habit, they only mention the infectious disease that triggered the sepsis—such as pneumonia—while failing to mention the sepsis. The reporting of causes of death and diagnosis codes for patients who have been hospitalized are affected by this issue.
Sepsis is underreported
So, just how common is sepsis?
One way to investigate the matter is to review patient records in retrospect to get a true picture. It is then possible to try to determine how many people actually had sepsis, regardless of the diagnosis they were given when they were treated.
According to a Swedish study, at least 500 in every 100,000 adults are hospitalized for sepsis every year. This means that at least 50,000 Swedish adults get sepsis every year. This includes the 3,000 to 5,000 people who develop septic shock, the more severe form.
According to the same study, the mortality rate from sepsis stands at around 17% in Sweden. This means that about 8,500 Swedes die from sepsis every year—almost ten times more than the number recorded in the National Board of Health and Welfare’s Cause of Death Register.
How can the diagnosis be uncertain when it comes to something so serious and yet so common?
According to the definition used in Swedish health care since 2018, sepsis is a condition involving life-threatening organ dysfunction caused by a disturbed systemic response to an infection.
Kristoffer Strålin explains, “Sepsis is always triggered by an acute infection. But the body’s response to this infection is excessive. We say that the host response—the body’s response, that is—is dysregulated, or incorrect. The body responds in a way that causes it to harm itself. This leads to organ failure, where one or more organs stop working. This is often life-threatening.”
This means that the pathways to sepsis can vary widely. An acute infection can be caused by almost any pathogen: bacteria, viruses, fungi or parasites. And the triggering infection could have originated anywhere in the body—in the respiratory tract, in the urinary tract or if chickenpox scars are scratched. Patients may then have vague symptoms that are easily confused with severe influenza.
So there is no typical process that can be communicated broadly in a message that is easy to understand. And when patients finally get to hospital, there is no simple test that can be done to detect sepsis.
Kristoffer Strålin has been responsible for developing what is known as a national sepsis care pathway, presented in 2021. Care pathways are commissioned by the Swedish Association of Local Authorities and Regions. They aim to make healthcare equal all over the country so that medical decisions are based on the same evidence.
A key element of the message about sepsis is that both the general public and healthcare professionals need to be better informed about the disease.
Facts: What everyone needs to know about sepsis
Who can get sepsis?
Everybody. But it is more common in people with fragile or compromised immune systems. This includes babies (especially premature babies), the elderly and people with cancer or other diseases that affect the immune system or require immunosuppressive treatment. Having recently given birth or having had surgery increases the risk, as does having had the spleen removed. This is also true in patients with an inlet such as a urinary catheter or venous catheter, or with a prosthesis or implant. Sepsis is slightly more common in men than in women, and the median age is about 80 years.
What are the signs of sepsis?
Acute onset of confusion or altered level of consciousness, shortness of breath, severe pain in the stomach, back, muscles or joints, diarrhea, vomiting, sudden onset of lethargy or muscle weakness (being unable to walk or stand), change in body temperature such as fever with or without chills or falling body temperature.
What should I do if anyone has these symptoms?
Phone 112. Say you suspect possible sepsis. Most people with sepsis who are taken to hospital get there by ambulance.
Furthermore, all A&E departments must have sepsis alarms. In short, this is a way of screening out suspected sepsis patients from the screening function already available at Swedish A&E departments. Today, patients are prioritized according to measured values for a range of vital signs, including blood pressure, respiratory rate and confusion. If a patient has high scores and an infection is present as well, that is when the sepsis alarm should be sounded.
Ding.
That is when the case is urgent. At Karolinska University Hospital in Huddinge, where there has been a sepsis alarm since 2017, a team of emergency doctors, infectious diseases doctors and intensive care doctors have to be on hand within fifteen minutes. The alarm sounds once a day, on average.
“The fact that we all arrive at the patient’s bedside at the same time and can discuss the case with each other and examine the patient together is a great advantage. It takes maybe fifteen minutes to half an hour. Then we all share a view of what we’re dealing with. For instance, the answer might be ‘yes, it’s sepsis and the infection seems to be in the urinary tract.’ Then we decide on which antibiotics to use depending to that,” says Kristoffer Strålin.
Six main organ systems or functions are affected by sepsis: lungs, liver, kidneys, brain, blood circulation (blood pressure) and blood clotting ability.
Respiratory rate, alertness, blood pressure, pulse rate and (possibly) decreased urine output are vital clues. A whole range of samples are also collected as specified by a predefined sepsis package. Some tests, such as those describing both blood oxygenation and renal function, provide answers within minutes. The C-reactive protein test, which reveals ongoing infection or inflammation, can also be carried out quickly. Other samples take longer to analyze.
The introduction of the new definition of sepsis in 2018 was accompanied by a new way of making the diagnosis. Findings related to the six organ systems are taken into account in a diagram. This results in a SOFA (sequential organ failure assessment) score, with at least two points required for diagnosis. The higher the score, the more severe the disease.
“These are patients who are monitored closely, with clinical assessments and new collection of samples. It’s common for us to admit a patient to the ward in the morning, observe a deterioration in their condition during the day and then transfer them to the ICU. And vice versa,” says Kristoffer Strålin.
More specific treatments are needed
But what treatment do these seriously ill patients receive? Can sepsis be cured?
Yes, it can. But there is no specific treatment for sepsis. Instead, it involves warding off the triggering infection with antibiotics and sometimes surgical interventions—draining an abscess, for example—and supporting failing organ functions. This includes administering fluids to maintain the blood pressure in vessels that have started to leak, giving oxygen, perhaps performing dialysis if the kidneys fail. And there are different levels of this kind of supportive treatment. Minor pulmonary effects can be supported with oxygen on a ward. More severe lung failure requires intubation with a ventilator and implies intensive care.
But not all patients survive sepsis, despite all the efforts made to save them. The mortality rate in Sweden has remained at about the same level for several years now, despite new diagnostic criteria that aim to identify more patients and attempts to increase the focus on the disease. Sepsis alarms are still being implemented all over Sweden.
“The fact that survival rates haven’t improved is because we administer the same treatment now that we did 20 years ago—organ support and antibiotics. We need treatments for the sepsis disease itself, for the false host response,” says Kristoffer Strålin.
There are drugs that affect the immune system in different ways. And there is some evidence to suggest that they may be effective in cases of sepsis. But only for some patients.
That is the key problem—sepsis patients differ so widely. More targeted and personalized treatment is needed to improve survival rates. The challenge rests in deciding who should have which treatment. People working at hospitals describe an enormous need for research and new knowledge in this regard.
One difficulty doctors have to deal with is that the immune system makes mistakes in several ways in cases of sepsis; both overreactions and underreactions.
Commonly, the pathogens causing the infection trigger a strong immune response. This leads to the release of many signaling substances, mainly cytokines, into the bloodstream. These then trigger chains of events that lead to severe inflammation in or around organs, such as inside blood vessels. Such extensive inflammation can cause organ failure. In these cases, the immune system needs to cool down.
Another scenario is when the immune system does not react positively enough. This may be due to attacks on the bone marrow, where many immune cells are produced. Other tentative attempts at explaining the matter suggest that the immune system is “exhausted”—it is unable to react potently enough to deal with the situation. Consequently, the patient is unable to protect themselves against new infections, which can result in new sepsis. This is a severe blow to an already damaged body, and in the worst case it can be fatal. In these cases, boosting the immune system would probably be valuable.
Some patients switch between the overreactive and the underreactive immune response.
But usually they occur simultaneously. One example is of a patient who arrives at A&E with a SOFA score indicating sepsis—but who has a low body temperature rather than a fever. For some reason, the body is unable to respond to the infection by increasing the temperature, even though the body has managed to create an excessive inflammatory response that harms vital organs—the host response is wrong in two ways.
The immune system may have stopped overreacting after a while. The patient has survived organ failure and should begin to recover. But then the underreaction might persist. The patient is then unable to defend against a new infection, which may result in a new sepsis. An even more serious one.
COVID-19 has led to new insights
It is difficult to conduct studies involving sepsis patients, partly because the group is so heterogeneous, as described: different pathogens cause the triggering infection, which may have started in different parts of the body.
However, the COVID-19 pandemic of recent years has made it possible to learn more.
“By definition, patients with severe COVID-19 have sepsis caused by COVID-19. They have a misregulated host response caused by a severe infection and more than two SOFA points. This condition could have been called COVID-19 with sepsis, but we have chosen to call it severe COVID-19,” says Kristoffer Strålin.
“As these patients are always infected with the same microorganism that always settles in the lungs, we have the opportunity to look for differences in the patients to help us understand which characteristics are associated with different disease processes,” says Kristoffer Strålin.
He is a researcher working on a European project involving Karolinska University Hospital. This project is evaluating a new rapid test indicating the function of the immune system in cases of sepsis. If the test is performed regularly on patients in ICU, it can at best provide an idea of how the body’s immune response seems to be evolving—is it scaling up, or winding down? The researchers hope that the rapid test could be a way in which to screen which patients need which treatment. Because drugs are available to use.
Cortisone is one example of a proven immunosuppressant. It has been used for a long time when caring for patients with septic shock, which is a serious and life-threatening form of sepsis. But the role of cortisone is contentious, because it is hard to know which patients will benefit from it. In some patients with septic shock and an overreactive immune response, cortisone can slow down what is known as the cytokine storm and thus reduce organ failure. At the same time, using cortisone in a patient who already has a suppressed immune response can have a direct negative impact on the progression of the disease and increase mortality, according to some studies.
Interferon is a drug that supports the immune system and has been used to treat certain cancers for a long time.
But again—who should be given what? And when?
Rapid tests may aid during dramatic events
One person who is hunting sepsis biomarkers is Professor Anna Norrby-Teglund, head of the Center for Infectious Medicine at the Department of Medicine, Huddinge.
She and her colleagues have examined blood plasma from sepsis patients where the infection has resulted in tissue damage, known as necrotising soft tissue infections, NSTIs. These are dramatic events where tissue death can occur within days or even hours, with the risk of amputation.
The researchers have identified thrombomodulin as a biomarker that identifies patients experiencing runaway infection. They have also found markers that identify patients who are at risk of developing septic shock.
“We want to go further and see whether we can develop a rapid test. We want to make it easier for doctors to recognize these patients quickly and admit them for surgery straight away,” says Anna Norrby-Teglund.
These necrotising soft tissue infections are often caused by group A streptococcus, a common bacterium that can cause tonsillitis, for example. Much of Anna Norrby-Teglund’s research focuses on group A streptococci.
They produce what are known as superantigens, substances that the immune system perceives as extremely provocative. Group A streptococci can activate up to 20 percent of our T-cells, a type of immune cell that learns to recognize specific pathogens. A more common immune response engages fewer than one percent of T cells.
These bacteria increase the risk of severe sepsis for everyone, even young, otherwise healthy people with an effective immune system. The large number of excited T-cells produces masses of cytokines. These kick-start the chaotic course of events.
Finding new treatments
Anna Norrby-Teglund has been researching a drug to use in this situation. This involves intravenous immunoglobulin, IVIG—or more precisely, immunoglobulin G, IgG. These are antibodies that are normally present in the bloodstream. They are currently given for certain diseases, and there is a procedure for separating them from donated blood plasma.
Researchers are using different tissue models to investigate the effect of IVIG. These are lab-constructed, three-dimensional models of lung, skin or other tissue.
The tissue models are created in the lab by growing cells from healthy individuals. They bear many similarities to real tissue and allow infection processes similar to those in cases of sepsis to be investigated. The researchers expose the tissue models to different bacteria and immune cells, sometimes adding different drugs. And then they watch what happens.
In these tissue models, treatment with IVIG has had good efficacy in superantigen infections.
“We’ve seen that the powerful T-cell response is absent when we stimulate the cells with superantigens and then add these antibodies. So it is effective.”
One major point is that all cells—both immune cells and bacteria—take on a more physiological behavior in the tissue models, explains Anna Norrby-Teglund. Among other things, this has provided answers to matters that were previously incomprehensible: how can live bacteria be hidden in tissue after just over a week of treatment with the right antibiotic?
Researchers have been able to see from tissue models that some bacteria form a protective biofilm around themselves. This does not happen if the bacteria are grown on glass or plastic, so in that environment they die because of the antibiotic.
When the bacteria’s protective shield was discovered, the researchers tested different combinations of antibiotics in the tissue models. Finally, they were able to identify a mix that breaks through the biofilm and kills the bacteria. This combination of antibiotics is now used at the clinic to treat sepsis.
“The tissue models are a more clinically relevant environment for the bacteria, it gives us a more accurate picture of how they behave. In this environment, we can try out potential treatments for different situations. Our aim is to understand the individual patient’s sepsis and tailor the treatment to the individual,” says Anna Norrby-Teglund.
Sepsis facts: Milestones
- Circa 400 BC: Hippocrates coined the term “sepsis.” The word means “decay” in classical Greek.
- 19th century: Robert Koch showed that specific bacteria cause specific diseases, which later earned him the Nobel Prize in Physiology or Medicine.
- 1913: William Osler identified the role of the immune system in cases of sepsis: “the patient seems to die because of the body’s response to the infection, rather than from [the infection itself].”
- 1928: Alexander Fleming discovered that antibiotics kill bacteria.
- 1953: Danish doctor Bjørn Ibsen opened the first intensive care unit in a converted classroom at Copenhagen Municipal Hospital.
- 2016: The current definition and diagnostic criteria, Sepsis-3, presented in the scientific journal JAMA, was introduced in Sweden in 2018.
Journal information:
Journal of the American Medical Association
Source: Read Full Article
