A study of immune-deficient adults and children has shown that patients who fail to respond positively to infections and vaccinations have robust humoral immunity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) structural proteins.
Researchers Hannah Kinoshita et al. described the clinical course, antibody, and T cell responses to SARS-CoV-2 structural proteins in a cohort of adult and pediatric patients with antibody deficiencies (related and unrelated) and infected with SARS-CoV-2. The researchers at Children's National Hospital are the first to demonstrate this response for immunocompromised patients. Their findings are published in the Journal of Clinical Immunology.
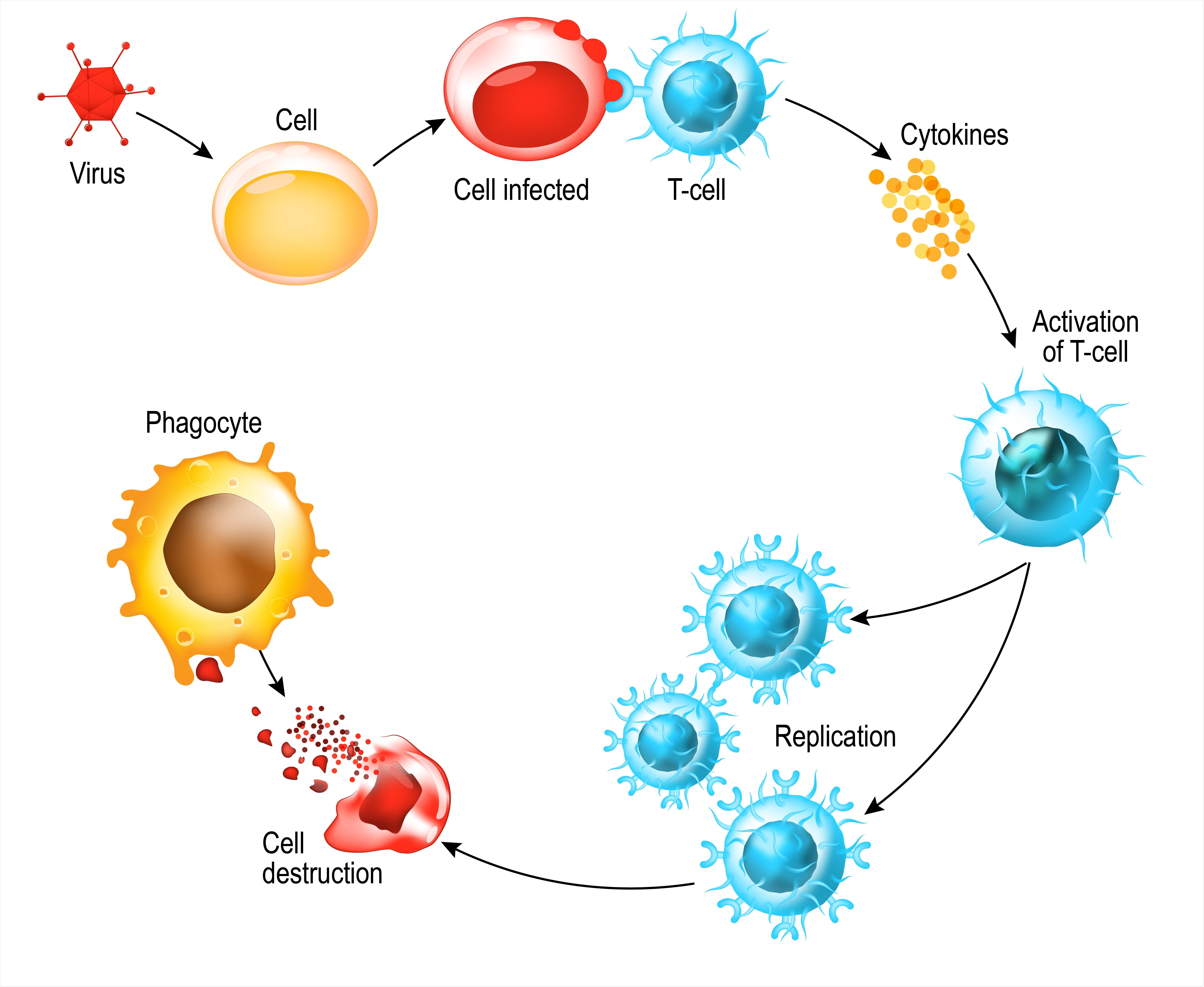
"Given the reliance on spike protein in most candidate vaccines, the responses are encouraging. If T-cell responses to SARS-CoV-2 are indeed protective, then it could suggest that adoptive T-cell immunotherapy might benefit more profoundly immunocompromised patients," said Michael Keller, M.D., director of the Translational Research Laboratory in the Program for Cell Enhancement and Technologies for Immunotherapy (CETI) at Children's National. "Through our developing phase I T-cell immunotherapy protocol, we intend to investigate if coronavirus-specific T-cells may be protective following bone marrow transplantation, as well as in other immunodeficient populations."
The study cohort included five patients within the same family – 3 with antibody deficiency and 2 immunocompetent controls (including a family group of three children and their mother). They showed antibody responses to the viral nucleocapsid and spike proteins, as well as the SARS-CoV-2 specific T cell immunity at days 65–84 from the onset of symptoms. The researchers took blood samples to test the T-cell response in cell cultures and provided comprehensive statistical analysis of the adaptive immune responses.
The control participants in the study were the father of the same family, who tested positive for COVID-19, and another incidental adult (not next of kin), who experienced mild COVID-19 symptoms. The researchers observed no significant difference between the immunocompromised patients and controls.
Additionally, the researchers assessed two unrelated adult patients with common variable immune deficiency. While one of them did not show antibody response, the researchers found that both demonstrated SARS-CoV-2-specific T cell immunity when evaluated 33 and 76 days, respectively, following SARS-CoV-2 diagnosis.
In antibody deficiency disorders, the protective immune responses to infections and vaccinations fail. Previous studies demonstrated that in immunocompromised patients, about 20% of the cohort required intensive care, with an overall mortality rate of 10%; 6 of 9 deceased patients suffered from an antibody defect.
These findings represent increased morbidity and mortality, especially at younger ages, compared with the general population. However, the current study, led by researchers at Children's National Hospital, provides a comprehensive analysis of the immune responses in these patients.
Thus, this study establishes that patients with antibody deficiency disorders, including inborn errors of immunity (IEI) and common variable immunodeficiency (CVID), can mount an immune response to SARS-CoV-2 – showing promise that vaccination may still be helpful for this population.
"This data suggests that many patients with antibody deficiency should be capable of responding to COVID-19 vaccines, and current studies at the National Institutes of Health and elsewhere are addressing whether those responses are likely to be protective and lasting," said Dr. Keller.
The researchers call for additional studies to further define the timing of onset of immunity, the longevity of the immune response, and the variability of response against SARS-CoV-2 in immunocompromised patients compared with healthy donors.
"This was a small group of patients, but given the high proportion of responses, it does suggest that many of our antibody deficient patients are likely to mount immune responses to SARS-CoV-2," said Dr. Keller. "Additional studies are needed to know whether other patients with primary immunodeficiency develop immunity following COVID-19 infection and will likely be answered by a large international collaboration organized by our collaborators at the Garvan Institute in Sydney."
- Kinoshita, H., Durkee-Shock, J., Jensen-Wachspress, M. et al. Robust Antibody and T Cell Responses to SARS-CoV-2 in Patients with Antibody Deficiency. J Clin Immunol (2021). https://doi.org/10.1007/s10875-021-01046-y
Posted in: Medical Research News | Disease/Infection News
Tags: Antibody, Blood, Bone, Bone Marrow, Cell, Children, Common Variable Immune Deficiency, Coronavirus, Coronavirus Disease COVID-19, Hospital, Immune Response, Immunodeficiency, Immunology, Immunotherapy, Intensive Care, Laboratory, Mortality, Protein, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, T-Cell

Written by
Dr. Ramya Dwivedi
Ramya has a Ph.D. in Biotechnology from the National Chemical Laboratories (CSIR-NCL), in Pune. Her work consisted of functionalizing nanoparticles with different molecules of biological interest, studying the reaction system and establishing useful applications.
Source: Read Full Article
