Several studies related to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) have shown that the virus adversely affects major organs, e.g., the central nervous system (CNS). SARS-CoV-2 is the causal agent of the ongoing coronavirus disease 2019 (COVID-19) pandemic, which has already infected more than 517 million individuals worldwide.
Background
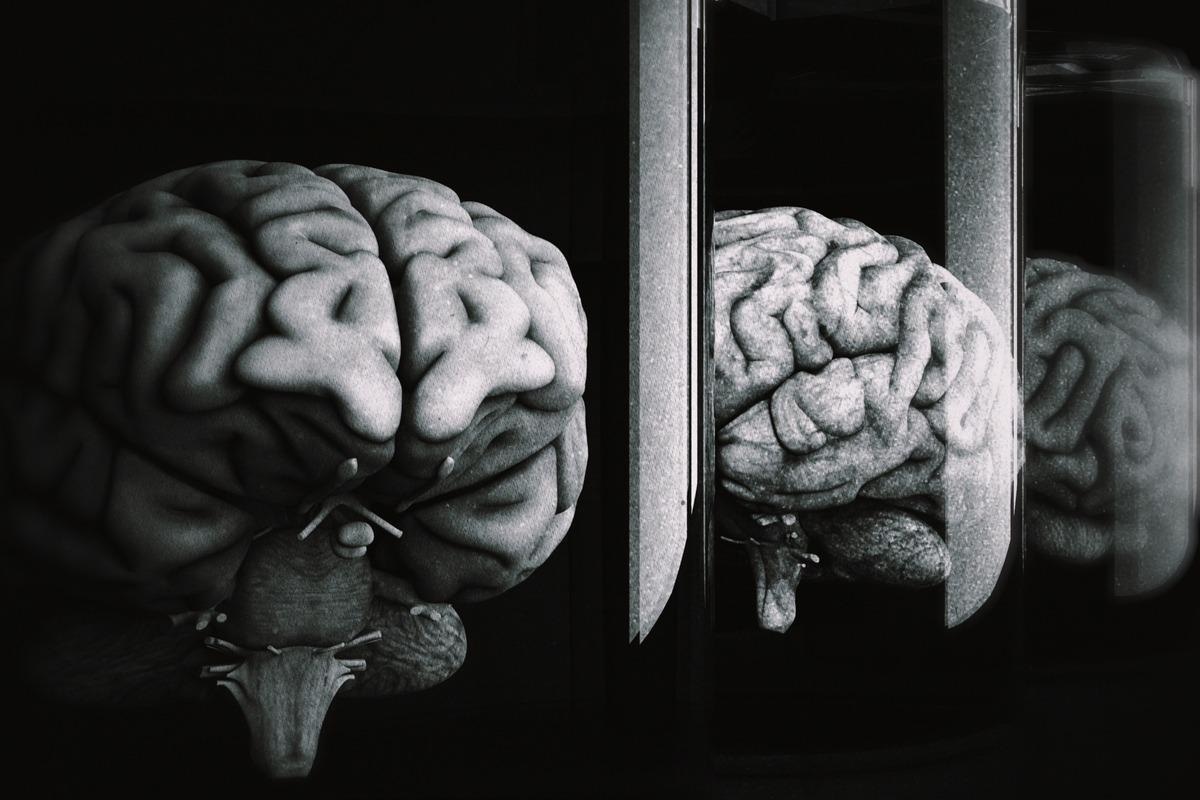
Previous studies have shown that COVID-19 disease causes CNS lesions associated with hemorrhage, encephalitis, encephalopathy, etc. Additionally, detection of SARS-CoV-2 proteins in the brain tissues via immunostaining suggested the presence of virions in the brain parenchyma as well as in the vascular endothelial cells.
Scientists have suggested that the introduction of CNS lesions in COVID-19 patients might have occurred due to SARS-CoV-2 invasion via olfactory apparatus or infection of vascular endothelial cells. Further, the CNS could also be indirectly damaged in COVID-19 patients through coagulopathy, hypoxia due to pulmonary disease, or dysregulation in the renin-angiotensin system (RAS) owing to the viral infection.
Prior research has also shown that cytokine storm or hypercytokinemia could cause CNS damage. Although several studies have indicated the indirect effect of COVID-19 on CNS, scarce evidence is available regarding the direct effect of SARS-CoV-2 on brain infection.
A new study
A new study currently posted to the Research Square* preprint server while under consideration for publication at the BMC Diagnostic Pathology has focused on the microcirculatory factors associated with neurological complications of COVID-19.
Researchers performed histopathology of the brains obtained from thirty-six consecutive autopsies of COVID-19 patients in the current study. All the study candidates showed positive RT-PCR for SARS-CoV-2. In the current study, immunostaining was conducted for serum proteins, complement components, and the virus. Additionally, researchers performed viral in situ hybridization studies. The authors used the Mann-Whitney U test to compare activation of complement in brain microvessels in COVID-19 samples with immunostaining findings of pre-pandemic autopsy brains.
Key findings
Scientists revealed that all thirty-six autopsy cases were of middle-aged to elderly adults. Both the genders were almost equally represented, and most of the candidates exhibited hypoxia. However, the clinical progression of the disease varied considerably in terms of length and complexity.
The majority of patients were hypertensive, and over half of the cohort had suffered from diabetes mellitus, obesity, chronic heart condition, and a history of cancer or pulmonary disease. Interestingly, over half of the cohort consisted of African American ethnicity. However, owing to the small size of the study cohort, ethnicity was not an influencing factor.
In the brain’s microcirculatory system, normal CNS blood vessels’ (microvessels and capillaries) diameter ranges between 40 and 400 µm. Previous studies indicated that although CNS microcirculation could not be directly detected via magnetic resonance imaging (MRI), specific imaging methods are able to procure brain microvasculopathy in COVID-19 patients.
In the current study, researchers reported the presence of both reactive and acute inflammatory microcirculatory alterations in all thirty-six COVID-19 autopsy cases. Previous research indicated some conditions that lead to microcirculatory injury from COVID-19, which were hypoxia, RAS dysfunction, and hypercytokinemia. A prior study linked CNS microcirculation with endocytosed pseudovirions, which might have been formed by SARS-CoV-2 protein and associated with vascular endothelial cells.
Researchers found many microscopic sections to be unusual, and the majority of the samples were distorted, dilated, and had thin-walled microcirculatory channels. Scientists stated that stalled microcirculatory healing in the brain during severe hypoxia might be enhanced by hypercytokinemia in COVID-19. Acute endotheliitis was found in half of the study cohort in two of the three major brain regions. Additionally, it was present in the brainstem of all but one patient.
Researchers stated that acute endotheliitis is an autoimmune vasculitis, which is present in the initial phase of type 3 hypersensitivity vasculitis. The finding of a previous study is consistent with the current study that revealed karyorrhectic polymorphonuclear leukocytes (PMNs) in autoimmune vasculitis led to the recruitment of mononuclear cells in small-vessel vasculitis.
Researchers reported that acute perivasculitis was present in 72.2% of the study cohort. They stated that more research is required to confirm the likelihood of circulating and planting SARS-CoV-2 proteins in the brain’s microcirculatory channels. Interestingly, 50% of the study cohort indicated induction of microcirculatory stress due to the presence of megakaryocytes in cerebral capillaries in COVID-19 cases.
Conclusion
The authors of this study reported the widespread prevalence of reactive and acute inflammatory CNS microvasculopathy in thirty-six COVID-19 brain autopsies. Owing to the scarce neurologic reports following hospitalization due to severe COVID-19 infection, scientists failed to provide the clinical correlation with histopathologic findings. However, previous findings indicated that hypoxia, hypercytokinemia, and RAS dysfunction have mostly caused reactive microvasculopathy in COVID-19 patients.
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Rhodes, R. et al. (2022) "Reactive and acute inflammatory microvasculopathy in 36 COVID-19 autopsy brains". Research Square. doi: 10.21203/rs.3.rs-1619440/v1. https://www.researchsquare.com/article/rs-1619440/v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Angiotensin, Blood, Blood Vessels, Brain, Cancer, Capillaries, Central Nervous System, Chronic, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, Diabetes, Diabetes Mellitus, Diagnostic, Encephalitis, Encephalopathy, Heart, Histopathology, Hybridization, Hypersensitivity, Hypoxia, Imaging, Magnetic Resonance Imaging, Nervous System, Obesity, Pandemic, Pathology, Protein, Renin, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stress, Syndrome, Vascular, Vasculitis, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
