Researchers at the National Institute of Standards and Technology (NIST) have built an online tool that could help decrease the concentration of aerosols containing the novel coronavirus in the hospital rooms of COVID-19 patients and other spaces such as offices, retail stores and residences, potentially reducing the likelihood of building occupants becoming infected.
The Fate and Transport of Indoor Microbiological Aerosols (FaTIMA) tool considers factors including ventilation, filtration and aerosol properties to estimate the concentration of aerosols a person might encounter in a room. Using the new tool, building managers and engineers can evaluate their options for reducing occupant exposure to the novel coronavirus. A new report serves as a FaTIMA user guide.
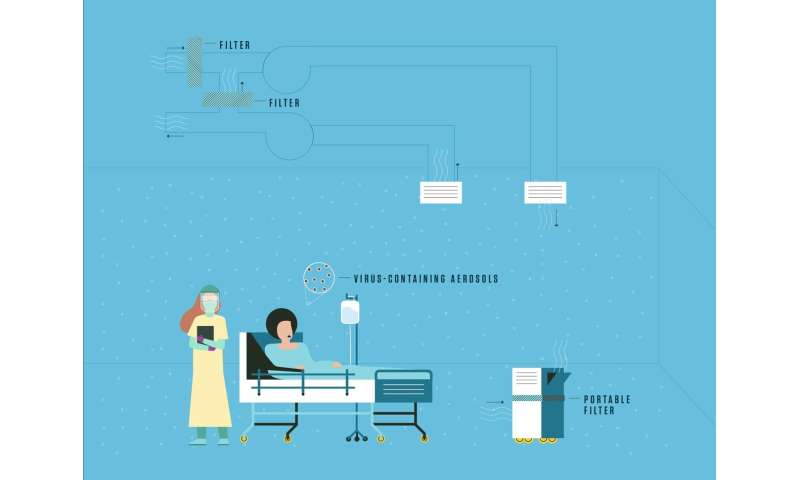
When people breathe, cough and sneeze, they release respiratory droplets and smaller aerosols less than five millionths of a meter in size. Compared with respiratory droplets, the smaller aerosols can remain in the air for longer periods of time. The current data suggest the novel coronavirus is primarily transmitted through contact with larger droplets, but tiny aerosols can also harbor the virus and may pose a threat to people, especially indoors. To establish a sound defense against these aerosols, informed management of airflow and airborne contaminants could be critical.
The researchers leveraged their expertise in developing airflow and contaminant transport models to build FaTIMA, which is based on the NIST software CONTAM.
“We have been developing CONTAM for decades, and it has been validated and verified for analyzing many aspects of building performance including indoor air quality,” said Stuart Dols, NIST mechanical engineer and a developer of FaTIMA.
CONTAM has been used to tackle a range of airflow issues in a wide variety of structures. To address the ongoing concern about airborne viruses, Dols used it to build a model of a single room. With FaTIMA, users can set the number of people in the room and the rate at which they exhale aerosols.
For FaTIMA to perform its calculations, the user must provide details about a room’s geometry, ventilation rates, air filter efficiencies and the presence of portable air cleaners, all of which can influence the concentration of small airborne particles to varying degrees.
The tool also requires specifics about the virus-containing aerosols, such as their size and how quickly they deposit onto surfaces. Although the properties of aerosols containing the novel coronavirus are not yet clearly defined, aerosols carrying the more well-studied influenza virus can be modeled in FaTIMA to approximate their behavior.
“The analysis in the tool is more about the aerosols, particularly their size, than the virus within them,” said Andrew Persily, chief of NIST’s Energy and Environment Division. “Most of the aerosol content is respiratory fluid, with the virus being a lesser part by mass and volume.”
The users are free to adjust the aerosol property inputs as they see fit, but by default, the values in the tool are based on previous studies of influenza-containing aerosols, which are referenced in the report.
FaTIMA can simulate an individual’s exposure for up to 24 hours even if the person only enters the room periodically, Dols said. In the case of a caregiver scheduled to check on a patient every hour during a 12-hour shift, the tool would be able to predict the person’s average, peak and total exposure in the patient’s room over the course of the entire shift. The tool would also estimate the number of aerosols that had landed on the floors, walls and other surfaces in the room.
To find out how to decrease exposure levels for uninfected occupants, several approaches can be taken.
“There are generally three means to reduce exposure to airborne indoor contaminants. You could remove or reduce the source, dilute the room air with clean ventilation or outdoor air, or remove the contaminants using a room air cleaner or local exhaust fan. This tool enables all of these means to be accounted for,” Dols said.
FaTIMA users can vary factors such as ventilation rates, air filter ratings and emission rates (to account for the effects of masks, for example) to identify approaches that reduce aerosol concentrations. Informed by the tool, building managers and engineers can then develop strategies and implement them in real buildings, producing a safer environment for occupants such as health care workers on the front line.
Source: Read Full Article
