Persistent gaps in life expectancy between Black and white Americans have been highlighted by the COVID-19 pandemic. Yet, this gap has narrowed by nearly 50% in three decades, largely due to improvements among Black Americans, according to a study published in the Proceedings of the National Academy of Sciences (PNAS).
Co-authored by researchers at Princeton University’s Center for Health and Wellbeing, the study analyzed data from 1990 to 2018 to compare mortality rates between Black and White Americans, through the lens of place. They also compared the United States with Europe to provide a benchmark comparison.
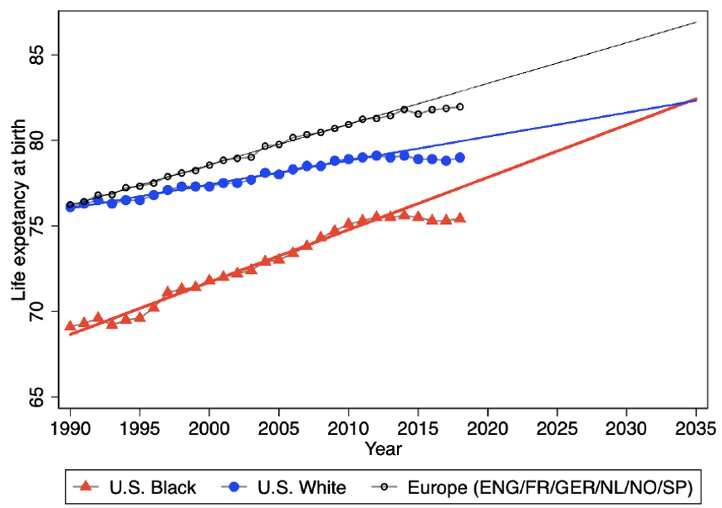
They found that in 1990, Black Americans lived seven years fewer than whites. But by 2018, that number had dropped to 3.6 years. Life-expectancy improvements in the poorest counties particularly helped narrow the gap, largely because Black Americans are more likely to live in the poorest areas. Reductions in Black deaths caused by cancer, HIV, homicide, and fetal and neonatal conditions were especially important in closing the gaps.
Yet, life expectancy has stalled for all groups in the United States since 2012, and, white Americans have lost ground relative to Europeans in both rich and poor areas. The U.S. opioid epidemic is one important cause of these declines, but the researchers suggest that more work should be done to investigate additional factors. If improvements had continued at the earlier rate, the racial gap in life expectancy would have closed by 2036.
“It is important to recognize the very real gains that have occurred over the past 30 years, and to understand the reasons for them” said Janet M. Currie, the Henry Putnam Professor of Economics and Public Affairs and co-director of Princeton’s Center for Health and Wellbeing. “Improved access to health care and safety-net programs all contributed to improvements in life expectancy among Black Americans. Yet, there is this perplexing reversal of the positive trends for all groups since 2012 that we need to better understand.”
Both the COVID-19 pandemic and the Black Lives Matter movement highlighted the disproportionate health gap between Black and white Americans, but the researchers wanted to quantify these differences in terms of trends in life expectancy in the years before the pandemic struck. To do this, they analyzed data from the National Vital Statistics System and the National Center for Health Statistics run by U.S. Centers for Disease Control and Prevention.
Their goal was to see whether racial differences in life expectancy have evolved differently in richer and poorer parts of the United States. They ranked American counties based on their poverty rates and placed them into groups of fixed population size. This allowed them to analyze trends across ages and race in places with the same relative poverty rates. Factoring in age is important in order to account for whether changes in life expectancy are based on a person’s stage of life; for example, people older than 65 qualify for Medicare, which could play a role in extending life expectancy.
They also wanted to understand how the United States compared to Europe to determine whether mortality in richer parts of the country is more similar to that of European countries, or whether both rich and poor Americans tend to lag behind. They collaborated with researchers in nine European countries, including Czech Republic, England, Finland, France, Germany, Netherlands, Norway, Portugal and Spain in order to analyze all of the data in a similar framework. These countries represent a range of economic conditions.
During the past three decades, white Americans have increasingly fallen behind Europeans. Within Europe, even relatively poor countries like Portugal, were able to catch up with richer countries by 2018 in terms of life expectancy, while the United States lagged behind. At the same time, life expectancy for Black Americans started far below both European and white American rates in 1990, but grew at a faster rate than European life expectancy.
Similar to the United States, European life expectancy also has stalled after 2014, suggesting that there may be a common element. Past work has linked the flattening of life expectancy in the U.S. to a lack of further improvement in the fight against cardiovascular disease, and this may also be true in Europe, the authors suggest.
Source: Read Full Article