A new paper in JNCI Cancer Spectrum, published by Oxford University Press, finds increases in both men and women for several HPV-related cancers in low-income counties or those with high smoking rates. Increases were slower in the highest-income US counties or those with low smoking rates.
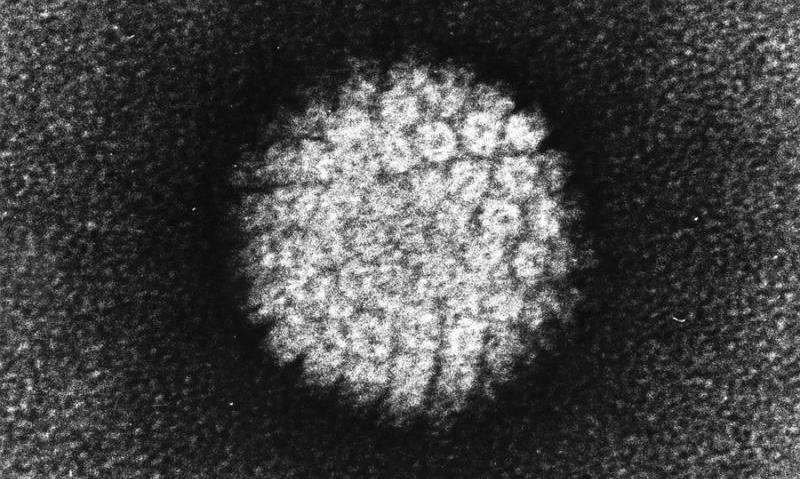
In the era of collective decline in cancer rates, human papillomavirus (HPV)-associated anal, oropharyngeal, and vulvar cancer is still rising. Risk factors for HPV-associated cancers include smoking and risky sexual activities, both behaviors likely more common in poorer parts of the United States.
Researchers here used the Surveillance, Epidemiology, and End Results database, a National Cancer Institute database that provides nationwide information on cancer statistics, to investigate HPV-associated cancers by US county-level income and smoking prevalence between 2000 and 2018.
They found that anal and vulvar cancer among women and anal cancer incidence among men increased significantly in the lowest-income counties and counties with high smoking rates, while the increases were slower in their counterparts.
Cervical cancer incidence plateaued, rising not at all in the highest income counties, but increasing 1.6% a year in the lowest income counties. Oropharyngeal cancer rates among women increased by 1.3% a year in low-income counties and only by .1% in high-income areas. Anal cancer rates among women increased by 3.2% in low-income counties but by only 2.6% in high-income areas. For vulvar cancer, rates increased 1.9% a year in the lowest-income counties but only vs. 0.8% a year in the highest-income counties. Vaginal cancer rates increased by 2% a year in low-income counties and declined by .3% in wealthier areas.
Among men, oropharyngeal cancer rates increased by 2.1% a year in low-income counties and by 1.7% per year in high-income counties. Anal cancer rates increased by 3.9% in low-income areas but increased by only 1.5% in high-income counties.
Counties with high smoking prevalence, which are also often low-income counties, had marked increases in cancer rates compared to their counterparts. Anal cancer among women increased by 5% a year for those living in high-smoking counties and only 1.9% a year for those living in lower smoking-rate counties. Vulvar cancer increased by 3.8% a year a year for those living in high-smoking counties and only .6% for those living in lower smoking-rate counties.
Oropharyngeal cancer rates among men increased by 2.7% a year in high-smoking areas, but only by 1.5% in low-smoking counties. Anal cancer incidence rates among men increased by 4.4% in high smoking-rate counties, but only by 1.2% in lower smoking-rate counties.
“HPV vaccination and cervical cancer screening are the cornerstone interventions to prevent avoidable suffering caused by six cancers,” said the study’s senior investigator, Ashish Deshmukh. “Unfortunately, cervical cancer screening rates declined in recent years and HPV vaccination rates remains 15% points lower in rural low-income counties. The COVID-19 pandemic has further disrupted the delivery of preventative care. Urgent and collective efforts are needed to prevent growing disparities from worsening.”
Source: Read Full Article
