In a world first, Newcastle researchers have discovered the mechanisms acute myeloid leukemia (AML) cells use to produce “free radicals”—the byproduct of a cell process that aggressively fuels the growth of cancer cells and limits the effectiveness of current treatments.
Published March 28 in Science Signaling, University of Newcastle and Hunter Medical Research Institute (HMRI) researchers also identified a strategy to silence the production of free radicals in leukemia cells, in turn strengthening their response to current therapies used to treat leukemia patients.
Reactive oxygen species (ROS)
The production of Reactive Oxygen Species (ROS), also known as free radicals, is a necessary and expected byproduct of cell processes within the human body.
However, overproduction or uncontrolled ROS can cause damage to DNA, cells and tissues, leading to disease.
In the case of cancer, malignant cells become addicted to ROS, using its destructive power to cause continual changes to cell growth and survival mechanisms, making them almost impossible to treat. Cancer cells also use ROS to amplify their growth through oxidation of proteins required for energy.
Biomedical scientist, University of Newcastle Associate Professor Mat Dun, said reports of excessive ROS in cancer had increased in frequency in recent years, however before now, the specific mechanisms involved, were poorly understood.
“We set out to investigate the source of ROS in leukemia cells and how ROS influences leukemia cell growth, survival and response to anti-cancer therapies.
“Importantly, we believed that if we could identify the way in which ROS was perpetuating the malignancy, we could find a way to mitigate ROS production and control or reduce leukemia cell growth and survival,” he said.
A global first
It is the first time the effect of ROS or free radicals has been characterized across the entire “proteome,” that is all proteins, in acute myeloid leukemia.
Associate Professor Dun said as ROS was believed to be a key player in almost all types of cancer, their discovery could potentially be effective for other types of cancer.
“Anti-cancer drugs typically work by targeting proteins, making our finding highly informative in leukemia research circles, which we hope will translate to improved survival for future leukemia patients.”
The journey to discovery
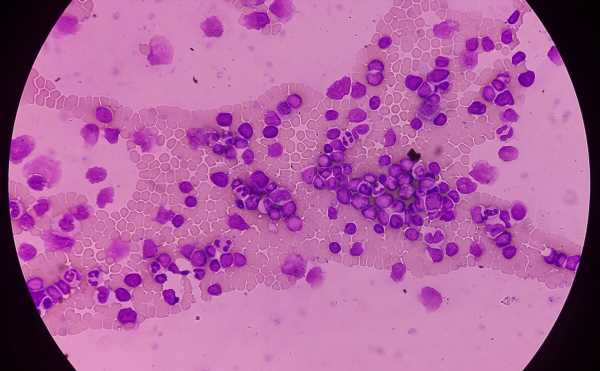
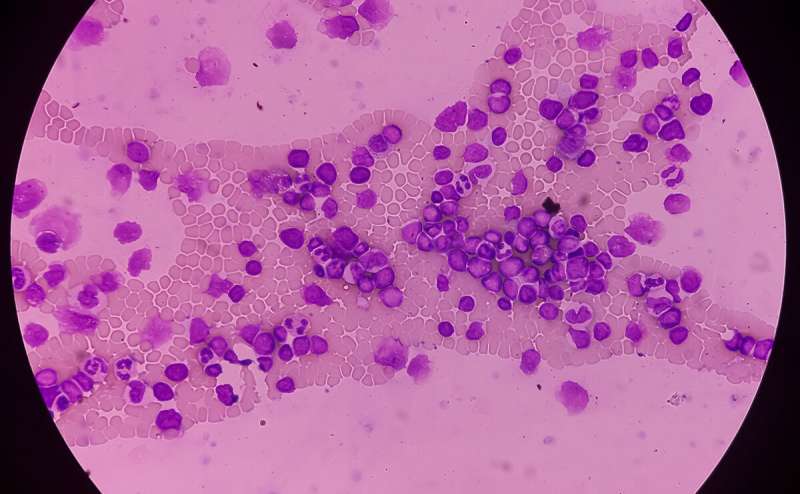
To conduct the research, the team used a specialist technique known as “high resolution proteomic profiling.” This involved assessing the range of proteins within blood cells from patients with acute myeloid leukemia versus healthy blood cells, as it is proteins that control how cells grow and respond to, or resist, cancer therapies.
With the help of their Danish collaborators, the team assessed how ROS influenced proteins within leukemia versus healthy cells.
“Our proteomic profiling showed that ROS-affected proteins were more highly expressed in some patients versus others, and, in those with high expression, we identified a genetic mutation common to each sample,” Associate Professor Dun explained.
Silencing of acute myeloid leukemia’s free radicals
Proteins identified as being affected in cancer samples are considered a therapeutic vulnerability.
“We knew if we could find or develop drugs that targeted the proteins active or present in the leukemia cells, we could impede the cancer’s ability to perpetually grow and survive.”
In partnership with pharmaceutical company GlaxoSmithKline, the team tested its novel, ROS-targeting drug in the leukemia models, discovering leukemia cell growth was impeded. This was particularly the case in models that mimicked drug-resistant types of leukemia.
“If future clinical trials confirm safety and effectiveness of the ROS-targeting drug, this approach will likely help a large subset of people with acute myeloid leukemia, including those with drug-resistant disease.”
More information:
Zacary P. Germon et al, Blockade of ROS production inhibits oncogenic signaling in acute myeloid leukemia and amplifies response to precision therapies, Science Signaling (2023). DOI: 10.1126/scisignal.abp9586
Journal information:
Science Signaling
Source: Read Full Article