A retrospective study led by Northwestern Medicine investigators found that the chimeric antigen receptor (CAR) T-cell immunotherapy drug tisagenlecleucel demonstrated safety and efficacy in pediatric patients with relapsed and refractory B-cell acute lymphoblastic leukemia (B-cell ALL), even when the drug doesn’t meet the FDA’s strict manufacturing standards.
The findings, published in Blood, may help widen therapeutic interventions for these patients who have otherwise exhausted all other treatment options, according to Jenna Rossoff, MD, instructor of Pediatrics in the Division of Hematology, Oncology and Stem Cell Transplantation and lead author of the study.
“I hope that these findings will make clinicians feel more comfortable with giving a slightly out-of-spec product to their patients, especially when they’re otherwise in a tight spot without other therapeutic options or ones with a very high toxicity profile,” said Rossoff, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
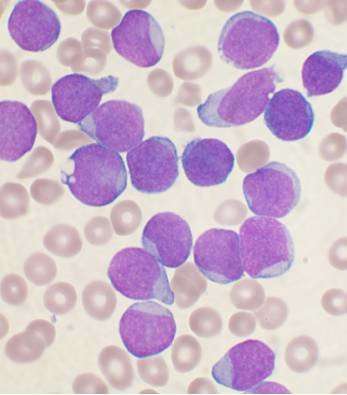
B-cell ALL, the most common type of cancer in children, is a type of blood and bone marrow cancer that develops in early forms of B-cells—white blood cells—and progresses quickly if left untreated. With the advancement of treatment, including chemotherapy, immunotherapy and radiation therapy, the five-year survival rate for pediatric patients with B-cell ALL has increased to 90 percent.
CAR T-cell therapy, a type of immunotherapy that utilizes a patient’s healthy T-cells that are collected through a process called leukapheresis and reengineered to attack cancer cells, has been shown to be especially effective for patients who have relapsed or are unresponsive to standard treatments.
A recent clinical trial found that pediatric patients with relapsed or high-risk B-cell ALL who received the CAR T-cell therapy drug tisagenlecleucel demonstrated a remission rate of 81 percent three months after infusion. Specifically, tisagenlecleucel utilizes a patient’s healthy T-cells that are reengineered to fight off the protein CD19 on the surface on B-cell ALL cancer cells.
While results from that clinical trial prompted the drug’s FDA approval in 2017, some of the FDA’s safety and efficacy specifications may be more stringent than necessary, according to the authors. Because of these criteria, some tisagenlecleucel is manufactured that fails to meet certain release criteria and is deemed ineligible for commercial release, or “out-of-specification.”
If a product is deemed out-of-specification, physicians can still decide to use the product, assuming there are no safety concerns. However, until now there has been little published data regarding clinical outcomes in patients with B-cell ALL who’ve received out-of-specification products, according to Rossoff.
In the current study, Rossoff and colleagues analyzed retrospective data from 185 pediatric patients diagnosed with relapsed or refractory B-ALL who received out-of-specification tisagenlecleucel or standard-of-care tisagenlecleucel at 15 pediatric clinical sites across the United States.
Overall, the investigators found that survival rates and toxicity profiles between both groups were similar, demonstrating the drug’s overall safety and efficacy.
In the future, Rossoff said more prospective studies performed in different clinical contexts are needed to create specific cut-off points that can help physicians more accurately determine which patients are will benefit from the therapy.
Source: Read Full Article