A team of experts, led by Glasgow Caledonian University (GCU) and the University of Bristol, in collaboration with NHS Tayside and the Scottish Drugs Forum (SDF), have just published a ‘game-changing’ blueprint on how best to get hepatitis C treatment to those who need it most after a successful three-year trial in NHS Tayside.
The breakthrough in getting treatment to those who inject drugs – studied as part of the National Institute for Health Research (NIHR)-funded EPIToPe (Evaluating the population impact of hepatitis C direct-acting antiviral treatment as prevention for PWID (people who inject drugs)) project – will help guide efforts in Scotland to eliminate hepatitis C by 2024.
Key recommendations include introducing a nurse-led community service for hepatitis C testing and treatment, recruiting peer workers who know the local drug culture and creating close ties between existing community services for people who inject drugs.
Researchers say the ideal model would be to house all these services in one building but where this is not possible the links between these services need to be strengthened including data sharing systems, role sharing and post-treatment care and support. A key part of that support is ongoing testing and treatment to prevent re-infection. It is hoped the guide will be rolled out across the UK and around the world.
The Scottish Government welcomed the findings and Public Health Minister Maree Todd said that “these recommendations will be a valuable resource as we continue to work towards our target of eliminating Hepatitis C in Scotland by 2024.”
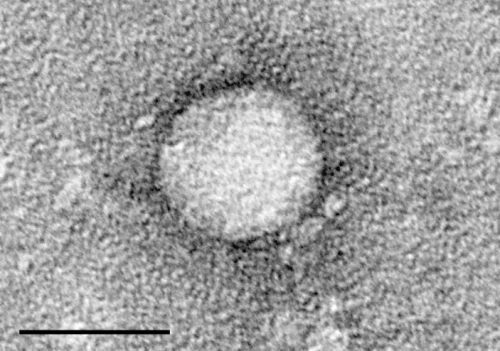
The hepatitis C virus (HCV) is a blood-borne disease that can seriously damage the liver and is spread mainly through blood-to-blood contact with an infected person. Despite effective Opioid Substitution Treatment and Needle Syringe Programmes, chronic hepatitis C prevalence remains at around 40% among people who inject drugs in the UK.
The World Health Organization (WHO) has set an elimination target to reduce hepatitis C transmission by 80 per cent and deaths by 65 per cent by 2030, and researchers believe this new method of getting treatment to those who inject drugs in communities will have a major impact on cutting incidence and death rates.
Lead GCU researchers behind the blueprint, Professor Lawrie Elliott, Dr Gabriele Vojt and Professor Paul Flowers, now at Strathclyde University, described the research as a “game changer in the design of hepatitis C treatment programs for those who inject drugs in Scotland and beyond.”
Professor Elliott added that they “know from previous research led by GCU that the treatment works but we have struggled to get this out to those who need it. These recommendations are a major breakthrough in getting treatment out to communities and will have a huge impact on virus elimination.”
EPIToPe study co-lead and GCU Professor of Epidemiology and Population Health Sharon Hutchinson, said that “the lessons learnt from the great strides made in NHS Tayside in tackling hepatitis C are captured in the set of recommendations. They have shown that it is feasible to deliver specialist nurse-led treatment across multiple community-based services engaged with people who inject drugs.
“The set of EPIToPe recommendations will help to guide other regions and countries in efforts to rapidly scale up hepatitis C treatment in this population, as is necessary to achieve the global WHO elimination targets.”
The study was co-led by Matt Hickman, Professor in Public Health and Epidemiology and co-Director of the NIHR Health Protection Research Unit in Behavioural Science and Evaluation at University of Bristol, and involved experts from the University of Dundee, Public Health Scotland, and NHS Bristol, North Somerset and South Gloucestershire, with the backing of drugs charities With You and The Hepatitis C Trust.
NHS Tayside Consultant Hepatologist and Gastroenterologist and University of Dundee Professor John Dillon said: “The goal of HCV elimination, removing the scourge of death and disease caused by HCV from our communities is within reach, but it needs coordinated action by all the players to achieve it. The recommendations are a useful tool to that end.”
Professor Hickman said scaling up hepatitis C testing and treatment in the community alongside harm reduction services was “critical” to prevention in the UK and achieving elimination targets.
“This is a very useful blueprint with practical suggestions for services and commissioners on how scale-up can be done – based on the successful transformation of services in NHS Tayside,” he added.
SDF CEO David Liddell welcomed the blueprint: “This type of assertive, responsive and inclusive approach to hepatitis C testing and treatment will go a long way to helping Scotland meet its 2024 elimination target.
“The recommendations have given us an evidence base for actions around which a consensus can readily be built as they will be consistent with the experiences of stakeholders delivering services.”
Source: Read Full Article
