Although it is quite hard to imagine a direct link between the intestinal microbiota and the central nervous system, a growing body of evidence indicates a bidirectional interaction between these two body systems. This is also known as the gut-brain axis.
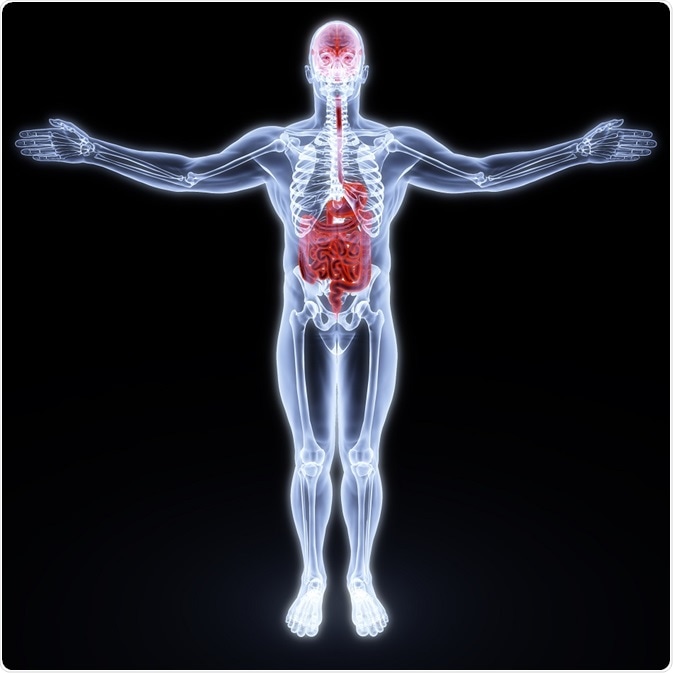
Credit: Dim Dimich/ Shutterstock.com
For decades the dominant paradigm in the medical literature was that microorganisms present in the gut are commensals that bring us benefits by keeping pathogenic bacteria at bay. More recent research demonstrates that these symbionts also have significant roles in helping us to digest food, produce essential metabolites and also in steering the development of the immune system.
Today we are becoming increasingly aware that gut microbiota plays a pivotal role in the brain development processes and brain functions.
The specificities of gut microbiota
The early postnatal period in humans is characterized by bacterial colonization, with the initial microbiota possessing a maternal signature. However, after one year of age the gut microbiota takes its adult form and remains there throughout life. As gut microbes can greatly influence all aspects of human physiology, they are often referred to collectively as the “living organ” or the “forgotten organ”.
In humans, the lower intestine contains between 1013 and 1014 microorganisms, with as many as one thousand distinct bacterial species and more than seven thousand bacterial strains. Moreover, the microbiota contains 150 times as many genes as the human genome. Thus it is not surprising that such a huge and diverse population can synthesize a plethora of bioactive agents.
The most prominent bacterial phyla are divided into two main phylotypes – Bacteroidetes and Firmicutes – and account for at least 75% of the microbiome. Other microorganisms found in the gut (albeit in reduced numbers) include Actinobacteria, Proteobacteria, Fusobacteria and Verrucomicrobia.
Dysbiosis (which is a term for microbial imbalance) may occur in some instances, and there is a growing amount of data that it can lead to both intestinal (such as inflammatory bowel disease and cancer) and extra-intestinal disease (such as metabolic syndrome, obesity, diabetes and atopy). Recent research has also shown that dysbiosis can be linked to neurological disorders, most notably Alzheimer’s and Parkinson’s diseases, autism and multiple sclerosis.
How can gut microbiota affect the brain?
At the moment, the precise mechanism of communication between the gut microbiota and brain circuits has not yet been fully elucidated. Gut microbiota generally exerts their effects on the brain not only via the nervous system (i.e. through the neuroanatomical pathway of the gut-brain axis), but also through the immune system, endocrine system and metabolic system.
The gut can interact with the brain by two neuroanatomical pathways. The first one represents a mutual information exchange system that uses direct links between gut and brain by means of the vagus nerve and the autonomic nervous system. The second one is a bidirectional communication system between the enteric nervous system in the gut, and vagus nerve plus the autonomic nervous system in the spinal cord.
Direct neural communication processes between the brain and gut microbiota are principally realized through the vagus nerve. Certain bacteria may stimulate the afferent neurons of the enteric nervous system, and the resulting vagal signals originating from the gut may induce anti-inflammatory responses, preventing infectious and inflammatory states that might otherwise be caused by pathological microorganisms.
Gut microbiota are also important in the development of the neuroendocrine system. For example, some gut bacteria can synthesize butyric acid, dopamine, serotonin and short-chain fatty acids, which influence the brain directly. Bacterial enzymes can also give rise to products such as ammonia or D-lactic acid which are neurotoxins. Furthermore, gut microbiota have the propensity to affect neural circuits related to the stress response.
Therefore, a myriad of vital neural influences in the human body are originated by the gut microbiota, with a subsequent influence on the whole organism – including the brain. This neuroactive capacity of the gut microbiota means that its modulation may well have immense therapeutic potential in a host of conditions.
Sources
- https://www.jci.org/articles/view/76304
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040025/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153777/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4359909/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458706/
- http://pubmedcentralcanada.ca/pmcc/articles/PMC4747781/
- Lyte M. Microbial Endocrinology and the Microbiota-Gut-Brain Axis. In: Lyte M, Cryan JF, editors. Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease. Springer, 2014; pp. 3-24.
Further Reading
- All Gut-Brain Axis Content
- Gut-Brain Axis and Neurodegenerative Disorders
- Gut-Brain Axis and Neuropsychological Disorders
- Gut-Brain Axis and Obesity
- Gut-Brain Axis and Psychobiotics
Last Updated: Feb 26, 2019

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article
