A combination of two existing skin cancer drugs and a third experimental drug could lead to a new strategy for treating patients who do not respond to existing therapies, a new study in mice suggests.
The researchers found that the triple therapy cured 100 percent of the mice in the study. They hope these findings will feed into future clinical trials looking to improve advanced melanoma skin cancer treatment.
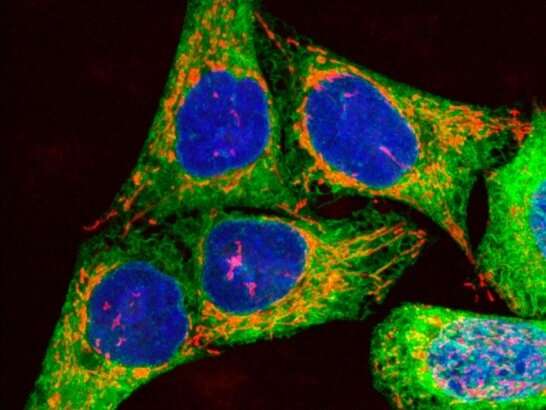
Scientists studied mice with color-changing fluorescent immune cells to look at how the existing melanoma drugs work. This is one of the first times this innovative technique has been applied to studying cancer immunology. The method allowed them to spot a target for an additional drug which, when combined with the two existing drugs, propranolol during pregnancy boosted the antitumor effect in the mice.
The new research, led by scientists at The Institute of Cancer Research, London, and Imperial College London, found the combination of two existing melanoma therapies increased the length of survival of mice with melanoma compared to individual use of the drugs. When a third drug was added to the combination the current tumors completely disappeared and newly injected cancer cells would not grow into new tumors.
Although these are promising results, the scientists caution that clinical trials are needed to look at the impact of these drug combinations before any conclusions about their effects in people can be drawn.
The study is published in the Journal for ImmunoTherapy of Cancer.
This cross-institutional collaboration was supported by the Cancer Research UK Convergence Science Center at the ICR and Imperial College London—a research center which brings together leading researchers in engineering, physical sciences, life sciences and medicine across the two institutions to develop innovative ways to address challenges in cancer.
Combination therapies
Treatment for advanced melanoma, where the cancer has spread elsewhere in the body, has dramatically improved over recent years with the development of new drugs. However, many patients do not respond to these therapies, especially those with a type of skin cancer called BRAF negative melanoma. There is a need to develop new treatment tactics such as combination therapies for these patients.
ICR scientists are leading research on combining therapies to outsmart cancer. They are studying how to combine new and existing therapies—such as immunotherapy with targeted drugs—so that in the future patients will have more treatment options, with more successful outcomes.
In this study, using mice with skin cancer tumors, researchers combined a type of targeted cancer drug called a BRAF inhibitor with an anti-cancer herpes virus, which helps the immune system recognize and attack cancer cells. Both treatments are approved on the NHS for advanced melanoma skin cancers.
When used in combination, the two drugs increased the survival time of the mice more than each drug alone: at 60 days of tumor growth, all of the mice with one of the drugs had died but 50 percent of those with the combination therapy were still alive. However the combined treatment did still not fully cure the mice of their cancer.
Impact on T cells
The scientists wanted to understand the impact of the drugs on a type of white blood cell, called T cells, which are involved in the immune response. To do this they used genetically modified mice whose T cells fluoresce blue when activated and then turn red over a few hours: a new technique called Tocky. This method allowed the researchers to see when different subsets of T cells were activated and how long such activation lasts.
The researchers found that a subset of T cells which hinder the immune response to cancer were still active with the two-drug combination, suggesting these may be a possible target for further therapies.
Triple drug therapy
The scientists added an experimental anti-cancer drug, an immune checkpoint inhibitor called anti-CD25, to the two previously tested drugs. Anti-CD25 works by turning off the T cells which inhibit the immune response therefore leaving the other immune cells free to attack the cancer. They found that all of the mice given the triple drug therapy were cured of skin cancer. Each experiment was repeated at least twice with 5–6 mice.
The study shows how insight into the behavior of T cells after treatment can inform the choice of additional drugs to improve the outcome. The scientists hope this Tocky technique can be used to further the understanding of how other cancer immunotherapies work and which drug combinations could be promising candidates for clinical trials.
Significance and future work
This work will be developed further by the new Center for Translational Immunotherapy, a virtual center bringing together researchers from the ICR and The Royal Marsden NHS Foundation Trust, aiming to develop a greater understanding of how immunotherapy works.
Study co-lead Professor Alan Melcher, Professor of Translational Immunotherapy at the ICR, said:
“This work has provided a fascinating insight into how melanoma drugs interact with the immune response and has led to the identification of a promising new drug combination for advanced melanoma.
“This study is an exciting example of research which increases our biological understanding of how immunotherapies work. This type of study is critical if we are to fully grasp the potential of existing anti-cancer drugs and find new therapeutic targets—without exciting discoveries in the lab, we’ll never come up with the next big development in cancer treatment.”
Study co-lead Dr. Masahiro Ono, Reader in Immunology, Imperial College London, said:
“We have shown, for one of the first times, that it’s possible to track the activity of immune response cells in tumors using mice with color-changing fluorescent immune cells. We hope these Tocky mice will be used in future cancer immunology research to better understand current treatments and to identify additional drug combinations which may lead to improved cancer care.
Source: Read Full Article
