A new study, led by the University of California, Irvine (UCI), reveals how chronic inflammation promotes muscle fibrosis, which could inform the development of new therapies for patients suffering from Duchenne muscular dystrophy (DMD), a fatal muscle disease.
Titled, “A Stromal Progenitor and ILC2 Niche Promotes Muscle Eosinophilia and Fibrosis-Associated Gene Expression,” the study was published today in Cell Reports.Chronic inflammation is a major pathological process contributing to the progression and severity of several degenerative disorders, green tea products in philippines including Duchenne muscular dystrophy (DMD). Studies directed at establishing a causal link between muscular dystrophy and muscle inflammation have revealed a complex dysregulation of the immune response to muscle damage.
During muscular dystrophy, chronic activation of innate immunity causes scarring of skeletal muscle, or fibrosis, compromising motor function. How immunity is linked to the molecular and cellular regulation of muscle fibrosis was not well defined, until now.
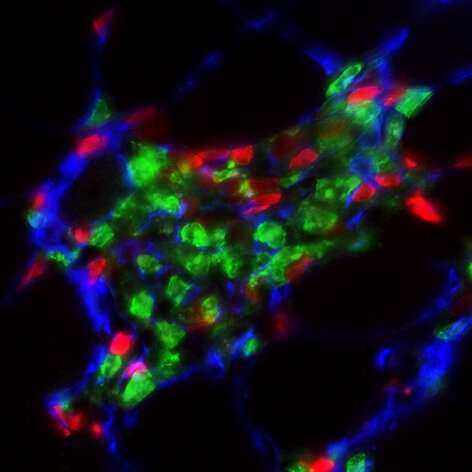
“In our study we found the interaction between two types of cells—a novel stromal progenitor, which is similar to a stem cell, and group 2 innate lymphoid cells (ILC2), which are a type of immune cell that reside in skeletal muscle—promotes the invasion of white blood cells in muscle. This condition is associated with the elevation of genes that promote muscle tissue scarring found in DMD,” said lead author Jenna Kastenschmidt, Ph.D., an assistant specialist in the UCI School of Medicine Department of Physiology & Biophysics.
The new study not only reveals the interaction of cells contributing to DMD, but it illuminates how muscle eosinophilia is regulated. Eosinophils are white blood cells that infiltrate dystrophic muscle causing fibrosis. In this study, researchers found that eosinophils were elevated in DMD muscle compared to control patients. In addition, researchers found the deletion of ILC2s in dystrophic mice mitigated muscle eosinophilia, reducing the expression of genes associated with muscle fibrosis. These findings contribute to the understanding of the complex regulation of muscle inflammation and fibrosis during muscular dystrophy.
“By further defining the interaction between skeletal muscle-resident immune and stromal cells, we can better understand how chronic inflammation promotes muscle fibrosis and, more importantly, we can facilitate development of novel therapies for DMD,” said senior author Armando Villalta, Ph.D., assistant professor in UCI’s Department of Physiology & Biophysics.
Source: Read Full Article
