Researchers sequenced the viral genome from samples in the state of Maharashtra and found a unique combination of three mutations that suggest the SARS-CoV-2 virus is continually evolving to evade the human immune response.
With the COVID-19 pandemic continuing to spread in several parts of the world, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is evolving to evade our immune system. Several new variants, cheap trazodone canada without prescription designated variants of concern, have been reported from the United Kingdom, South Africa, and Brazil at the end of 2020, which seem to be more infectious than the original strain.
The introduction of new variants and their consequences is important in guiding public health response in a country. With the tremendous spike in COVID-19 seen in India, especially in the state of Maharashtra, the government increased the sequencing of the viral genome to identify possible new mutants and understand the fitness of new strains.
Researchers from several Indian institutes involved in SARS-CoV-2 research obtained samples from international travelers to Maharashtra. About 5% of the surveillance samples tested positive and were sequenced, and the whole genomes of SARS-CoV-2 analyzed.
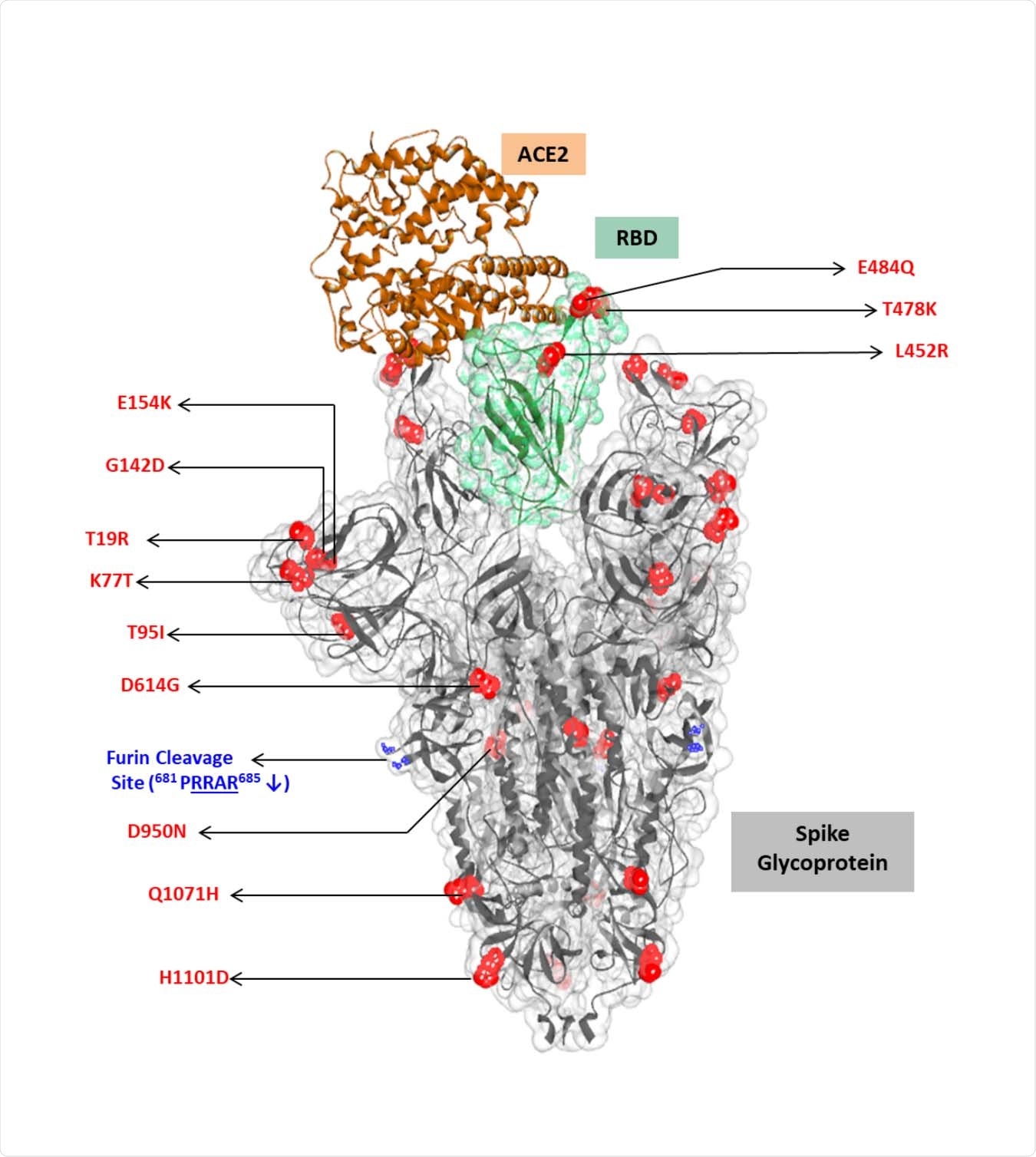
The team also analyzed the crystal structure of the top 10 virus spike protein mutations complexed with the human receptor, angiotensin-converting enzyme 2 (ACE2). They also assessed the effect of mutations on binding to two neutralizing antibodies using the structures.
Identifying mutations
After analyzing 598 whole viral genomes, the team found 47 G lineages. The most common was the B.1.617, which was found in about half the genomes sequenced. Within the B.1.617 clade, they found four clusters linked to specific spike protein mutations.
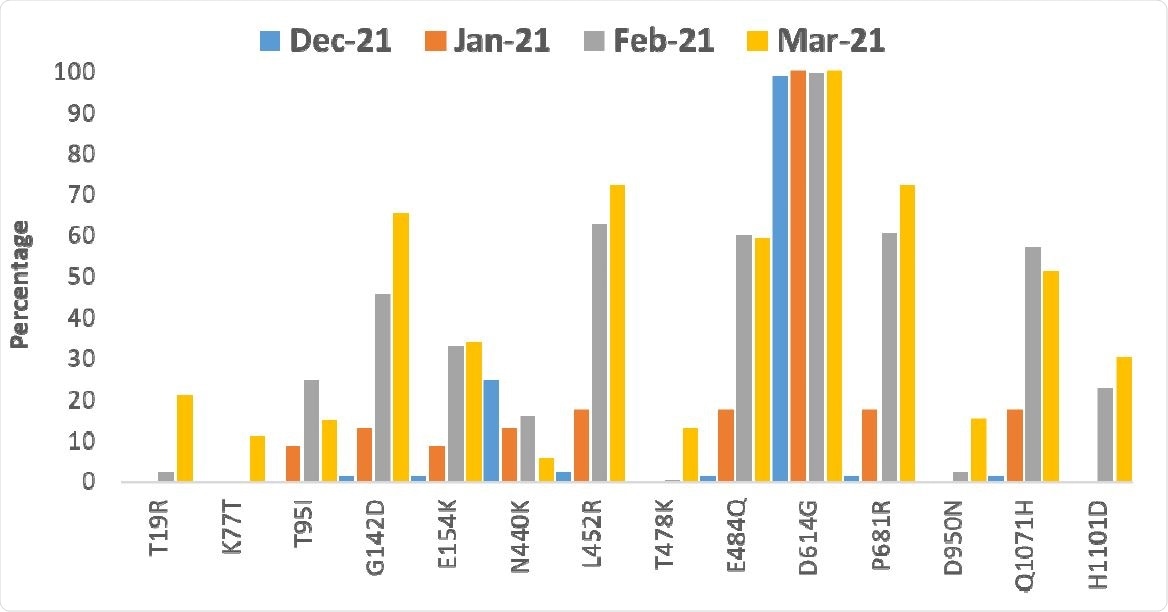
They found that mutations L452R and E484Q in the receptor-binding domain (RBD) of the spike protein and the mutations G142D and P681R outside the RBD increased in frequency from January 2021. Other mutations included H1101D and T95I. Only a small proportion of the sequences showed the B.1.1.7 variant, particularly in December 2020.
One cluster of mutations did not include E484Q and had T19R and D950N mutations in the spike protein. Another mutation D111D, occurred along with the RBD mutations L452R and E484Q but was not seen in the cluster without the E484Q mutation. Analysis indicated an increase in the frequency of non-synonymous mutations (those that change protein sequences) since February 2021.
In western Maharashtra, places such as Mumbai, Pune, Thane, and Nashik showed several lineages apart from the dominant B.1.617 seen in the eastern part of the state.
Mutations change interactions with ACE2 and antibodies
The crystal structure of the ACE2 complex with the spike protein suggests the mutations L452R and E484Q reduce intermolecular and intramolecular interactions compared to the wild-type virus. The L452R mutation removes the hydrophobic interactions with other nearby residues. But, the change from hydrophobic L452 to hydrophilic 452R increases the stability of the complex, likely because of its greater interaction with water molecules.
The E484Q mutation disrupts an electrostatic bond in the RBD. The mutation P681R in the furin cleavage site could help increased membrane fusion and thus cause increased transmissibility.
Both the mutations L452R and E484Q disrupt the interaction of the REGN10933 and P2B-2F6 neutralizing antibodies with the spike protein, thus reducing their neutralization effect.
Previous studies have shown that the L452R mutation reduces the neutralizing activity of several monoclonal antibodies, including those under clinical trials. This mutation can also escape cellular immunity, increasing viral infectivity and perhaps increase viral replication. Thus, this double mutant combination could escape monoclonal antibodies, requiring further studies.
Triple mutation
Mutations at sites 452 and 484 have been reported individually, for example, in the California variants B.1.427 and B.1.429, which have the L452R mutation. E484K has been seen in the variants reported from the United Kingdom, South Africa, and Brazil. Mutations at site P681 have also been seen in some lineages before as well as the mutation E484Q. The combination of all the three mutations reported here, L452R, E484Q, and P681R, suggests the virus is evolving similar traits independently, continually adapting to its human hosts.
The exponential increase in Maharashtra cases may be linked to this triple mutation and other spike mutations. Although the B.1.617 lineage has been reported in many other countries, its emergence locally needs continued monitoring to understand its impact.
The researchers conclude, ‘the study investigated the S protein mutations associated with the COVID19 cases in Maharashtra observed since the month of February 2021. The continuous increase in positivity could be attributed to signature mutations in the spike protein and functionally significant co-occurring triple mutations. As per GISAID submissions, the B.1.617 lineage has been reported from several countries, including UK, USA, Switzerland, Germany, Singapore, etc. However, the emergence of such local variants during the COVID19 second wave in India needs to be further investigated for their public health impact and its possibility of becoming a VOC.’
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Cherian S. et al. (2021) Convergent evolution of SARS-CoV-2 spike mutations, L452R, E484Q and P681R, in the second wave of COVID-19 in Maharashtra, India. bioRxiv, https://doi.org/10.1101/2021.04.22.440932, https://www.biorxiv.org/content/10.1101/2021.04.22.440932v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Coronavirus, Coronavirus Disease COVID-19, Enzyme, Frequency, Genome, Glycoprotein, Immune Response, Immune System, Mutation, Pandemic, Protein, Public Health, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Lakshmi Supriya
Lakshmi Supriya got her BSc in Industrial Chemistry from IIT Kharagpur (India) and a Ph.D. in Polymer Science and Engineering from Virginia Tech (USA).
Source: Read Full Article
