When they started the open biopsy, surgeons didn’t know what they were going to find, but they certainly didn’t expect this.
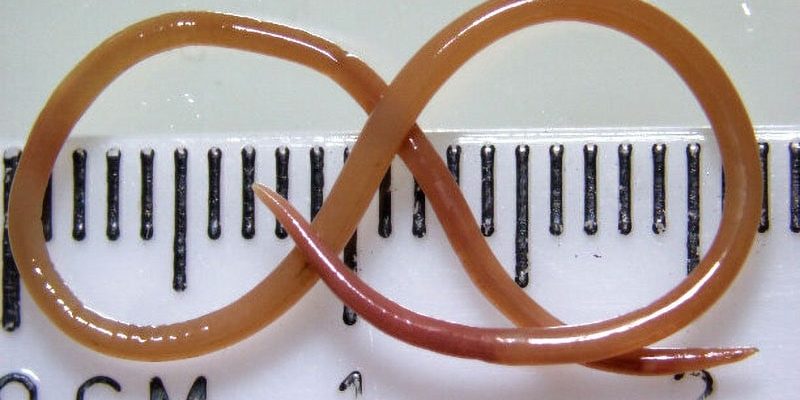
The stringlike worm was five sixteenths of an inch long, was alive, and wiggled.
“It stunned everyone in that operating theater,” says Sanjaya Senanayake, MBBS, an associate professor of infectious disease at Australian National University, Canberra, Australia, and senior author of the case report told Medscape Medical News. “When you operate on a brain, you don’t expect to find anything alive.”
The parasitic worm was about half the width of a dime. Helminths like it can usually be seen with the naked eye, but are often found in the intestines after being transmitted by soil and infecting the gastrointestinal tract. But this one made it into a woman’s brain in a first-of-its-kind case reported in the journal Emerging Infectious Diseases.
“We weren’t suspecting a worm at all,” Senanayake said. “There was something abnormal there. Was it going to be granulomatous lesion? Was it going to be cancer? Who knows, but it needed to be biopsied, and a worm was the last thing at the back of anyone’s mind,” he said.
A Year of Inexplicable Symptoms
The 64-year-old woman was diagnosed with pneumonia and had a high white blood cell count, low hemoglobin, high platelets, and a very high C-reactive protein of 102 mg/L.
She hadn’t fully recovered from her illness when the abdominal pain and diarrhea started. And then she had a dry cough and night sweats.
After 3 weeks of discomfort, she was admitted to the hospital. She had a history of diabetes, hypothyroidism, and depression and doctors began looking for answers to her acute illness.
They tested for autoimmune diseases and parasitic infections and prescribed prednisolone to help ease symptoms.
But 3 weeks later, her fever and cough persisted, and she was readmitted to the hospital. Doctors ordered more tests, and her eosinophils were still high, plus there were lesions on her liver, spleen, and lungs.
But tests were negative for bacterial, fungal, and mycobacterial cultures. Her stools showed no evidence of parasites.
She was prescribed mycophenolate and then ivermectin in case her tests for roundworm were a false negative. Doctors suspected Strongyloides, but lesions remained on her spleen even as the liver and lung lesions improved.
Reducing the prednisolone dose affected respiratory symptoms, so by January 2022, a year after initial symptoms began, the medical team added the monoclonal antibody mepolizumab. But her symptoms worsened, and she developed forgetfulness and more depression.
After a brain MRI revealed a right frontal lobe lesion, the team recommended an open biopsy and discovered the worm.
The specimen was Ophidascaris robertsi, the intestinal roundworm typically of the carpet python. Never before seen in a human, the only other animals in its life cycle are small marsupials or mammals consumed by pythons.
A Snake’s Bug
Although this is the first case of an Ophidascaris infection in a human, other cases could occur, warn the doctors in their case report.
The best guess for how the patient contracted the infection was by inadvertently consuming larval eggs on wild vegetation that she collected near her home to eat. She lived near a lake known to be home to carpet pythons, so the eggs could have been on the plants she collected or on her hands or kitchen equipment.
“If you’re foraging or using native grasses or plants in recipes, it would be a good idea to cook those instead of having a salad,” Senanayake said. “That would make the chance of getting something really rare even less likely.”
It’s unclear how or why the worm, which usually stays in the gut, made its way into the patient’s brain, but her long course of immunosuppressing drugs may have played a role, the team points out. “If the normal immune barriers are reduced, then it’s easier for the parasite to move around between organ systems,” Senanayake said.
Doctors also wondered if she may have been getting re-infected when she went home between hospital admissions? After removing the worm, she received 4 weeks of treatment with albendazole to eliminate any other possible larvae in other organs, especially since Ophidascaris larvae have been known to survive for long periods — more than 4 years in laboratory rats. “The hope is that she’s been cured of this parasitic infection,” Senanayake said.
As people around the world contend with the global COVID pandemic, they might not realize that new infections are arising around the world every year, he explained.
Novel Parasitic Infections
“The reality is that 30 new infections appeared in the last 30 years, and three quarters of them are zoonotic, animal infections spilling over into the human world,” Senanayake said.
Though some of those infections are the result of improved surveillance and diagnostics, a real increase has been occurring as human settlements continue expanding.
“This is just a reflection of how burgeoning human populations are encroaching upon animal habitats, and we’re getting more interactions between humans and wild animals, domestic animals and wild animals, and humans and natural flora, which is increasing the risk of this type of infection being recognized,” he explained.
The Ophidascaris worm found in this instance is in other snake species in different continents around the world, too. “Awareness of this case will hopefully lead to the diagnosis and treatment of other cases,” Senanayake added.
Though it’s certainly surprising to find this particular parasite in a human, finding a zoonotic organism in a person isn’t that strange, according to Janet Foley, DVM, PhD, a professor of veterinary medicine at the University of California, Davis. This is especially true if the usual host is closely related to humans, like primates, or spends a lot of time around them, like rats.
“There are still a lot of parasites and diseases out there in wildlife that haven’t been discovered and we don’t know the risk,” said Foley. “But still, the risk would have to be low generally or we would see more human cases.”
In the United States, the roundworm common in raccoon feces is Baylisascaris procyonis and can be dangerous for people. “There have been deaths in people exposed to these worms, which do seem to prefer to travel to a human brain,” Foley said.
A 2016 Centers for Disease Control and Prevention report described seven US cases identified between May 2013 and December 2015, including six that caused central nervous system disease. Another case report in 2018 involved a toddler who had eaten dirt and animal feces in his backyard.
And this past June, an Emerging Infectious Diseases case report described a B. procyonis infection in a 7-year-old with autism spectrum disorder and a history of pica. He had put material in his mouth from the ground near a tree where epidemiologists later found raccoon feces.
Still, Senanayake cautions against people jumping to conclusions about parasitic infections when they experience symptoms that aren’t otherwise immediately explainable.
The typical person who develops forgetfulness, depression, and a fever probably doesn’t have a worm in their brain or need an immediate MRI, he pointed out. “There may be other cases out there, but common things happen commonly, and this is likely to be rare,” Senanayake said.
This case demonstrates the challenge in picking a course of treatment when the differential diagnoses for hypereosinophilic syndromes is so broad.
Tricky Hypereosinophilic Syndromes
One of those differentials for the syndromes is parasitic infections, for which treatment would be antiparasitic agents, but another differential is an autoimmune condition that would call for immunosuppression.
“Obviously, as with this case, you don’t want to give someone immunosuppressive treatment if they’ve got a parasite, so you want to look really hard for a parasite before you start them on immunosuppressive treatment for an immunological condition,” Senanayake said.
But all the blood tests for different antibodies came back negative for parasites, “and this parasite was simply difficult to find until they pulled it from her brain,” he said.
Infectious disease physicians are always looking for the unusual and exotic, Senanayake explained. But it’s important to exclude the common, easy things first, he added. It’s after exhausting all the likely culprits that “you have to start really thinking laterally and putting resources into unusual tests.”
For more news, follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube.
Source: Read Full Article