Early studies of COVID-19 focused on the acute phase of the disease. However, attention has now turned to the long-term consequences of the disease, which are also significant causes of morbidity and mortality.
Two studies reported in The American Journal of Pathology seek to understand the drivers of the chronic and sometimes progressive phase of the disease and identify possible pathways for drug treatment.
The COVID-19 pandemic has highlighted the need to better understand both acute and chronic disease triggered by severe respiratory viral infection. The acute phase of disease with severe pneumonia and lung injury dominated early management efforts and research priorities. However, progressive and often long-term disease is also a significant cause of morbidity and mortality.
A high percentage of patients with COVID-19 survived the acute infectious illness only to experience a considerable degree of organ dysfunction over a more prolonged period during and after initial hospitalization.
In the first study highlighted here, investigators deliver a roadmap for the pathogenesis of post-viral lung disease and the basis for a drug therapy for long-term COVID-19 and related post-viral conditions. In the second study, investigators used a hamster model of human COVID-19 to study the cause of coagulation abnormalities and microscopic indicators of pulmonary vascular damage associated with severe cases of COVID-19 in humans.
Results showed indirect vascular damage, possibly secondary to immune dysfunction, to be a major contributor to vascular damage, suggesting that novel therapeutics targeting the dysregulated immune system may prove effective.
In the study led by Michael J. Holtzman, MD, Pulmonary and Critical Care Medicine, Department of Medicine, and Department of Cell Biology and Physiology, Washington University School of Medicine, Saint Louis, investigators examined a series of autopsies of patients performed long after COVID-19 onset.
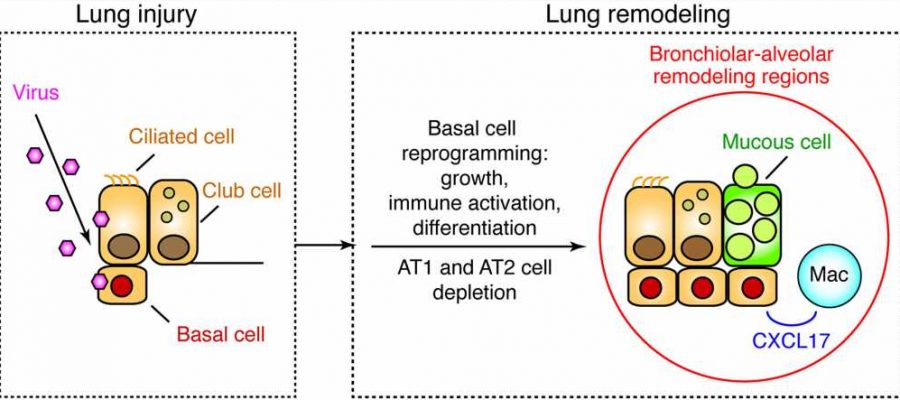
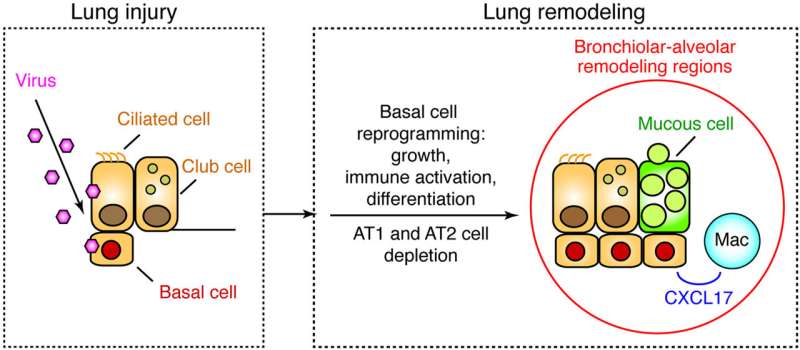
Dr. Holtzman explained, “Our research was inspired by the pressing need to understand the COVID-19 crisis, and especially to define the cause of the disease. We examined a series of consecutive fatal cases that came to autopsy between 27 and 51 days after hospital admission. In each patient, we identified a stereotyped bronchiolar-alveolar pattern of lung remodeling with basal epithelial cell hyperplasia, immune activation, and mucinous differentiation.”
“Remodeling regions also featured macrophage infiltration and apoptosis and a marked depletion of alveolar type 1 and 2 epithelial cells. This pattern was very similar to our experimental models of progressive lung disease after respiratory viral infection.”
The investigators noted several key scientific impacts based on identifying remodeling regions with basal epithelial cell hyperplasia and metaplasia extending into former alveolar spaces; concomitant dropout of both types of alveolar epithelial cells normally found in these spaces; epithelial stem-progenitor cell differentiation to mucous cells with a mixture of mucosal and submucosal types of mucin production; and macrophage infiltration linked to basal epithelial cell-specific chemokine production.
Dr. Holtzman commented, “Taken together with the results of our previously published animal models of post-viral lung disease, these studies deliver a roadmap for the pathogenesis of post-viral lung disease and the basis for a disease-modifying strategy for long-term COVID-19 and related post-viral conditions. The research defines a pattern of disease that implicates specific cell and molecular targets for therapy. Indeed, we are now developing a drug therapy that aims precisely at fixing those targets.”
As the pandemic progressed, physicians frequently reported clinical evidence of coagulation abnormalities and microscopic indicators of pulmonary vascular damage associated with severe human cases of COVID-19, noted Erin E. Ball, DVM, Ph.D., Department of Pathology, Microbiology, and Immunology, University of California, Davis, and colleagues.
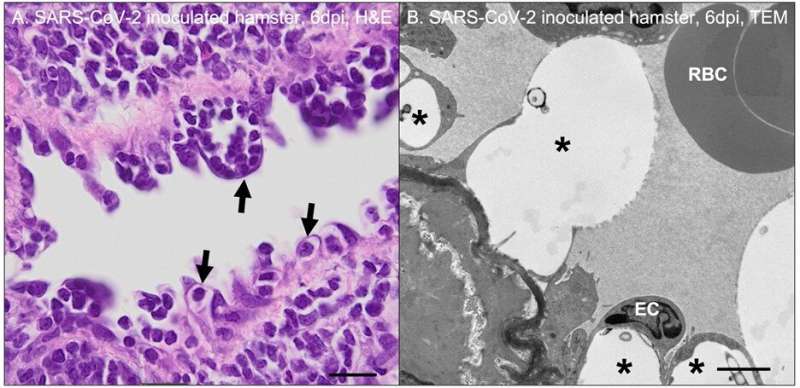
A team of investigators led by Dr. Ball injected severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) that causes COVID-19 into a Syrian golden hamster model of human COVID-19 to determine the cause of pulmonary vascular damage. At three to seven days post inoculation, they detected SARS-CoV-2 antigen and RNA within airway epithelial cells, pneumocytes, and macrophages, but not associated with blood vessels.
Their results showed that regions of active pulmonary inflammation in SARS-CoV-2 infection were characterized by ultrastructural evidence of endothelial damage with platelet marginalization and perivascular and subendothelial macrophage infiltration. SARS-CoV-2 antigen or RNA was not detectable within affected blood vessels.
The investigators had initially assumed the prominent microscopic vascular lesions noted in hamsters between three and seven days post SARS-CoV-2 inoculation would be the result of direct viral infection of cells comprising blood vessels; however, this was not the case.
Dr. Ball added, “These findings suggest that indirect vascular damage, possibly secondary to immune dysfunction, is a major contributor to vascular damage observed in SARS-CoV-2-inoculated hamsters and potentially severe COVID-19 infection in humans. Immune dysregulation resulting in excessive production of pro-inflammatory cytokines, endothelial damage, and platelet hyperactivation is a plausible driving force behind the hypercoagulable state and microthrombosis observed in some COVID-19 patients.”
Although this was an observational study, these findings, and particularly the lack of viral association with inflamed vessels together with published data, collectively support a primarily indirect mechanism linking inflammation and hypercoagulability in severe cases of COVID-19. These results suggest that novel therapeutics targeting the dysregulated immune system may prove effective medical countermeasures against COVID-19.
More information:
Kangyun Wu et al, Lung Remodeling Regions in Long-Term Coronavirus Disease 2019 Feature Basal Epithelial Cell Reprogramming, The American Journal of Pathology (2023). DOI: 10.1016/j.ajpath.2023.02.005
Erin E. Ball et al, Severe Acute Respiratory Syndrome Coronavirus 2 Vasculopathy in a Syrian Golden Hamster Model, The American Journal of Pathology (2023). DOI: 10.1016/j.ajpath.2023.02.013
Journal information:
American Journal of Pathology
Source: Read Full Article