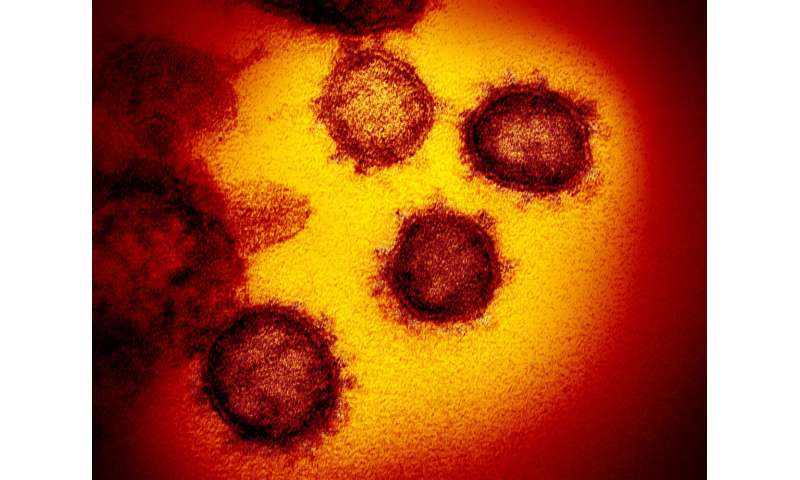
The COVID-19 pandemic has impacted virtually every aspect of cancer care and research- from introducing new risks for cancer patients to disrupting the delivery of cancer treatment and the continuity of cancer research, a review of scientific literature shows. The report, by researchers at Dana-Farber Cancer Institute and other institutions, suggests that while COVID-19 has complicated the treatment of cancer patients, it has also spurred creative solutions to challenges in clinical care, and research into the new disease is benefiting from insights gained over years of cancer research.
While much remains to be learned about the intersection of cancer and COVID-19, the new paper, published online by Cancer Cell, represents the most comprehensive survey to date about what physicians have learned, and what research is suggesting, about the interrelationship between the two diseases, the authors say.
“COVID-19 has been responsible for killing more than one million people worldwide. Among those most at risk of developing severe forms of the illness are patients with cancer,” says Ziad Bakouny, MD, MSc, of Dana-Farber, the co-lead author of the study with Jessica Hawley, MD, of Columbia University Medical Center. “Research into why patients with cancer are at heightened risk is moving very quickly. In this paper, we look at the state of the science in this area and others related to these two illnesses.”
The paper summarizes findings in four areas: the interconnected biology of cancer and COVID-19; changes in patient care prompted by the pandemic; effects on cancer research; and insights from cancer research applicable to the treatment of COVID-19.
COVID-19 and cancer biology
In patients with cancer, COVID-19 can be especially harsh. This is likely because many patients have a weakened immune system—either as a result of the cancer itself or the therapies used to treat it—and are therefore less able to fight off infection by the novel coronavirus. Several studies have examined whether systemic cancer therapies such as chemotherapy and targeted therapies increase patients’ vulnerability to COVID-19. The results so far are mixed, Bakouny says, possibly because such studies have focused on systemic therapies as a group rather than on specific agents. Future studies will attempt to tease out the effects of particular drugs.
One of the most dangerous consequences of COVID-19 is an overaggressive immune response known as a “cytokine storm,” which can damage lung and other tissues. Patients with cancer treated with immune-stimulating therapies such as immune checkpoint inhibitors, chimeric antigen receptor (CAR) T-cell therapies and bi-specific T-cell engagers (BiTEs) are at risk for complications if the immune response produced by these therapies results in an attack on normal, healthy tissue. Patients treated with CAR T-cell therapies and BiTEs, in particular, can develop a side effect known as cytokine release syndrome, which is similar to the cytokine storm in patients with COVID-19. Researchers have theorized that COVID-19 could exacerbate cytokine release syndrome in patients treated with certain immunotherapies, but studies have not definitely shown that this is happening, the new report states.
Although patients may be understandably concerned about facing an increased risk from COVID-19 as a result of cancer therapy, they shouldn’t let this deter them from seeking treatment for their cancer, Bakouny says. “Therapies for cancer can prolong life and even be curative in many cases,” he remarks. “It’s very important to be mindful of the goals of therapy and discuss with your doctor the risks and benefits of therapy in your own particular case.”
COVID-19 and cancer care
Around the world, efforts to thwart the spread of COVID-19 included steps to decrease in-person visits between patients and physicians. Among these was a jump in the use of telemedicine, which, some studies indicate, can be just as effective as in-person meetings. One study involving patients with breast cancer found that telehealth was associated with a higher quality of life and less depression and distress compared with usual care. While virtual visits offer a variety of benefits—less need to travel to physician appointments and incur the costs and inconvenience associated with travel—they’re valuable only insofar as they don’t take the place of in-person visits for exams, treatment, or diagnosis, research shows.
“It is also important to consider the unintended consequences of widespread adoption of technology,” Bakouny says. “There is a serious potential risk of compounding health disparities between patients of different socioeconomic status, if telehealth services are mandated.”
On the negative side, studies have shown a sharp decline in cancer diagnoses and screening during the peak of the pandemic. One study found that routine screening dropped by 85-90%. Delays in diagnosing cancer are likely to have long-term ripple effects. A British study estimates that, because of diagnostic delays, deaths five years from now may be 4-17% higher, depending on tumor type, than they would have been had the pandemic not occurred.
COVID-19 and cancer research
To limit the opportunities for viral transmission, many research centers enacted policies limiting the number of lab workers allowed on-site, putting many studies on hold. For the most part, research projects funded by government appropriations have not been hobbled by the pandemic, but some projects supported by private philanthropy face a funding gap. COVID-19 has drastically decreased donations to cancer-focused philanthropic organizations. The American Cancer Society, for example, expects a $200 million decrease in donations this year and has not been able to accept applications for research grants for the Fall grant cycle.
Clinical cancer research, in which potential new therapies are tested in patients, has also experienced difficulties as a result of COVID-19. Some cancer centers halted enrollment on clinical trials entirely during the height of the pandemic. A survey of dozens of clinical investigators in March found that nearly 60% of respondents had halted screening and/or enrollment in certain trials, and that half of their institutions had ceased collection of blood and other tissue for research purposes.
Despite these challenges, investigators found a variety of ways to adapt to straitened circumstances so trials could continue. These included leveraging telehealth to limit in-person visits, use of e-signatures for trial documentation, shipping oral medications to trial participants rather than requiring them to be picked up at the clinic, and allowing laboratory tests to be done at outside labs.
“The relaxation of some of the regulatory requirements associated with clinical research has been accomplished without compromising patient safety,” Bakouny remarks. “Many investigators see this as a plus—something that could be part of clinical research going forward, to reduce the cost of trials and facilitate the arrival of new therapies for patients.”
COVID-19 and lessons from cancer
Some promising approaches to treating COVID-19 have come, perhaps surprisingly, from cancer research, the paper’s authors write. While cancer and COVID-19 are fundamentally different in their origin, development, and effect on the body, some of the insights gained in decades of research in cancer are showing relevance to fighting the new coronavirus.
A variety of drugs used to alleviate cytokine release syndrome in cancer patients are being evaluated for effectiveness against cytokine storm in patients with COVID-19. Other drugs in the anti-cancer arsenal are undergoing tests of their potential value against COVID-19. An example is acalabrutinib, which is used in the treatment of lymphoid cancers. In one trial, it resulted in rapid improvements in oxygen requirements and a sharp drop in inflammation in patients with COVID-19.
Another potential point of connection between cancer and COVID-19 involves a protein called TMPRSS2. When the coronavirus is breathed in, it binds to lung cells and is split by TMPRSS2, allowing it to enter and infect the cells. Research has shown that in prostate cancer, TMPRSS2 is regulated by the androgen receptor, a cell structure that signals the cell to grow in response to androgen. The androgen receptor is found not only on prostate cells but on cells of the lung as well. It isn’t clear yet whether the receptor regulates TMPRSS2 in lung tissue, but if it does, it could open the way to a new treatment for COVID-19. Androgen-targeting therapies already used to treat prostate cancer could block TMPRSS2 from entering lung cells, preventing COVID-19 at its source.
Source: Read Full Article
