According to a manuscript published in the American Journal of Roentgenology (AJR), lacking Medicare coverage could contribute to greater income-based differences in use of screening CT colonography (CTC) than of other recommended screening strategies or of diagnostic CTC.
Noting that Medicare’s non-coverage for screening CTC may account for lower adherence with screening guidelines among lower-income beneficiaries, “Medicare coverage of CTC could reduce income-based disparities for individuals avoiding optical colonoscopy due to invasiveness, need for anesthesia, or complication risk,” concluded first author Eric W. Christensen, Ph.D., from the Harvey L. Neiman Health Policy Institute in Reston, VA.
Christensen et al’s AJR manuscript used CMS Research Identifiable Files—which contain claim information for 5% of Medicare fee-for-service beneficiaries—from January 1, 2011 to December 31, 2020.
Extracting individuals 45–85 years old, excluding those with high CRC risk, models were then constructed to determine likelihood of undergoing CRC screening (as well as the CMS-covered test with similar access: diagnostic CTC) as a function of income, race and ethnicity, and urbanicity. Data were controlled for sex, age, Charlson comorbidity index, U.S. census region, screening year, and related conditions and procedures.
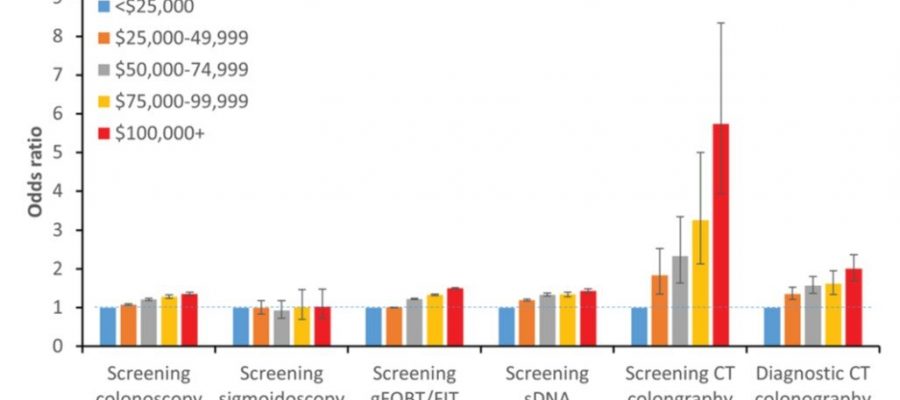
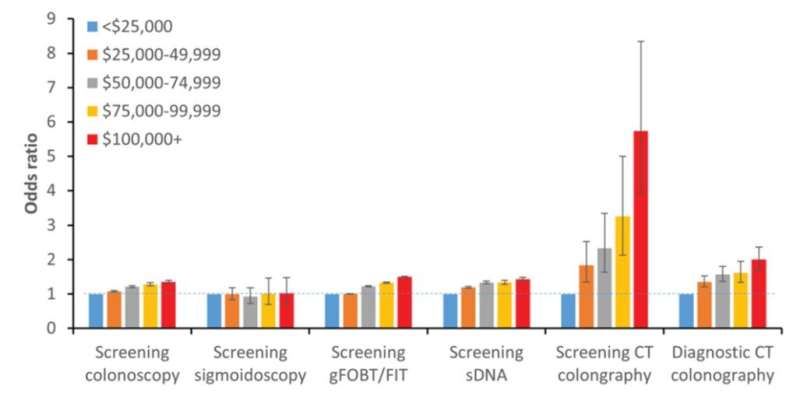
Ultimately, compared with Medicare beneficiaries in communities where per capita income was under $25,000 when controlling for race and ethnicity, those in communities with income greater than or equal to $100,000 were 5.7 times more likely to undergo screening CTC. Notably, this was a larger difference than observed for other CRC screening strategies (odds ratio, 1.03–1.50) or for diagnostic CTC (odds ratio, 2.00).
More information:
Eric W. Christensen et al, Sociodemographic Factors and Screening CT Colonography Use Among Medicare Beneficiaries, American Journal of Roentgenology (2023). DOI: 10.2214/AJR.23.29703
Journal information:
American Journal of Roentgenology
Source: Read Full Article