If either you or your partner was a “big” baby, you have an increased likelihood of giving birth to a large baby yourself, a new study by researchers from the University of Bergen, Norway, shows. This could potentially improve prenatal care and interventions by identifying pregnancies at higher risk of obstetric complications during labor and delivery.
The study from Norway explored the connection between parent’s own birthweight and the risk of having a big baby, and to what extent maternal body-mass index (kg/m2) (BMI) in early pregnancy also contributes to this risk. Exploiting the Medical Birth Registry of Norway, the oldest in the world, the researchers combined information on parent’s own birthweight to pregnancies they parented.
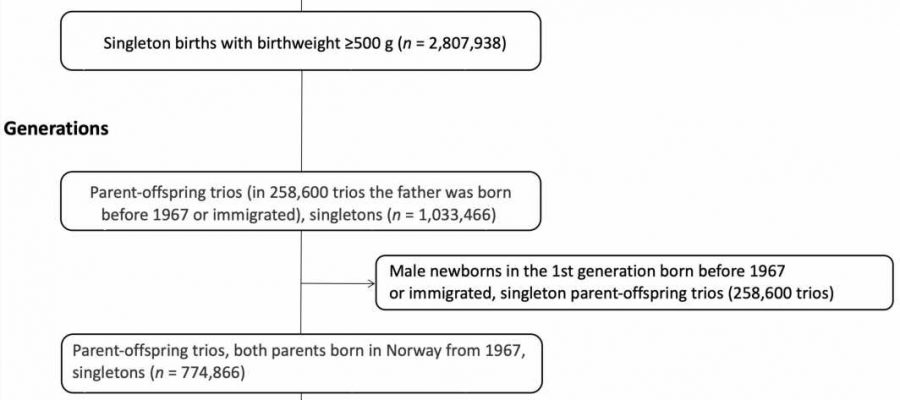
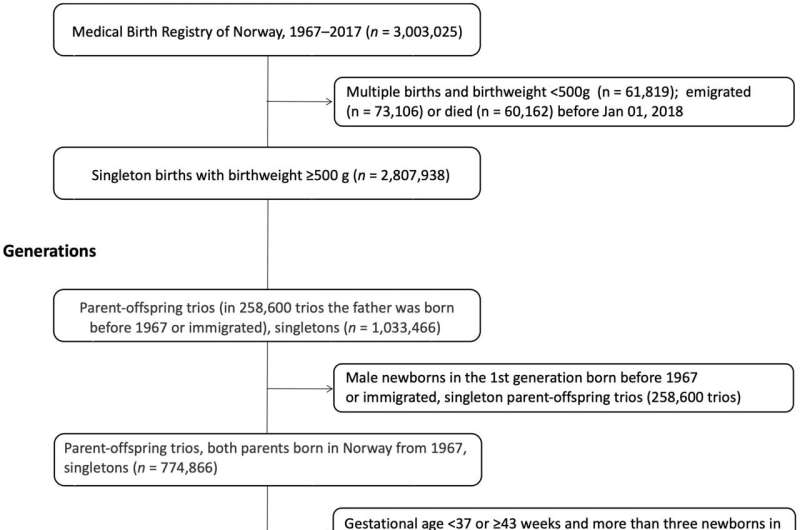
Parents and offspring born during a 50-year period were included, resulting in information on 647,957 births with available information on both parents’ birthweight. The study included only singleton newborns carried to term. Macrosomia, the scientific word for a “big” baby, was defined as a newborn weighing 4500 grams or more, and was more common among the offspring generation, with 4.0% compared to 3.2% among the parent generation.
The risk of giving birth to a macrosomic infant was much higher if the parents themselves were big at birth. Compared to both parents weighing below 4500 grams, there was a more than 6-fold increase if both had been big. Even with only one parent being macrosomic, the risk was more than double if the father had been macrosomic (relative risk 2.2) and more than 3 times if the mother only had been macrosomic (3.4).
The researchers also explored whether maternal BMI at the beginning of pregnancy contributed to the risk of birthing a macrosomic baby. The proportion of macrosomic newborns varied substantially by maternal BMI. Among the group where both parents had been born macrosomic, the proportion of babies also being macrosomic ranged from 17% when born to women who were normal weight before pregnancy (BMI 18.5-24.9), to 31% among women who was obese (BMI of 30 or more).
“Birthing a baby who is macrosomic comes with an increased risk of obstetric complications,” researcher Cathrine Ebbing says.
“One could speculate that through evolutionary mechanisms if the parent was big, this would protect the mother and child against macrosomia-related complications. However, we did not find that this risk was substantially diminished if the parents had also been born macrosomic,” Ebbing says.
This study adds another piece to the puzzle regarding the generational effect of birth outcomes, as well as the contributing effect of maternal BMI. The new insight may lead to new opportunities to detect pregnancies at risk of giving birth to a macrosomic child, and thus lead to more targeted prenatal care and interventions. However, further studies are required to examine the clinical usefulness of these predictions.
The work is published in the journal Paediatric and Perinatal Epidemiology.
More information:
Svein Rasmussen et al, Paternal and maternal birthweight and offspring risk of macrosomia at term gestations: A nationwide population study, Paediatric and Perinatal Epidemiology (2023). DOI: 10.1111/ppe.13005
Journal information:
Paediatric and Perinatal Epidemiology
Source: Read Full Article