In a recent study posted to the bioRxiv* pre-print server, researchers described a case of co-infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants of concern (VOCs)-Delta and Omicron.
The team identified a SARS-CoV-2 Delta-Omicron recombinant in an immunosuppressed kidney transplant patient who was treated with the neutralizing antibody (nAb)-sotrovimab after contracting coronavirus disease 2019 (COVID-19) for the first time in December 2021.
Notably, in December 2021, the Delta prevalence had declined to 10%, and that of Omicron had surged to 90% in New York, United States.
Background
In immunocompromised individuals, prolonged viral clearance allows the virus to evolve and form recombinants. Although a direct causative link was missing; presumably, sotrovimab exerted immune pressure leading to E340D mutation within the Omicron part of the SARS-CoV-2 spike (S) protein. Therefore, the following three possibilities arose –
i) the recombinant escaped sotrovimab treatment in a Delta/Omicron co-infection,
ii) the recombinant had replication advantages, or
iii) the patient contracted the recombinant from an unidentified source.
Clinical background of the patient
The patient was a male with end-stage renal disease due to hypertensive nephrosclerosis. He underwent a kidney transplant surgery in June 2021 and started with his immunosuppressive regimen. The patient received thymoglobulin at the time of transplant, later, for maintenance, he received tacrolimus, prednisone, and mycophenolate mofetil, and his concurrent medications included nifedipine, labetalol, pantoprazole, and entecavir.
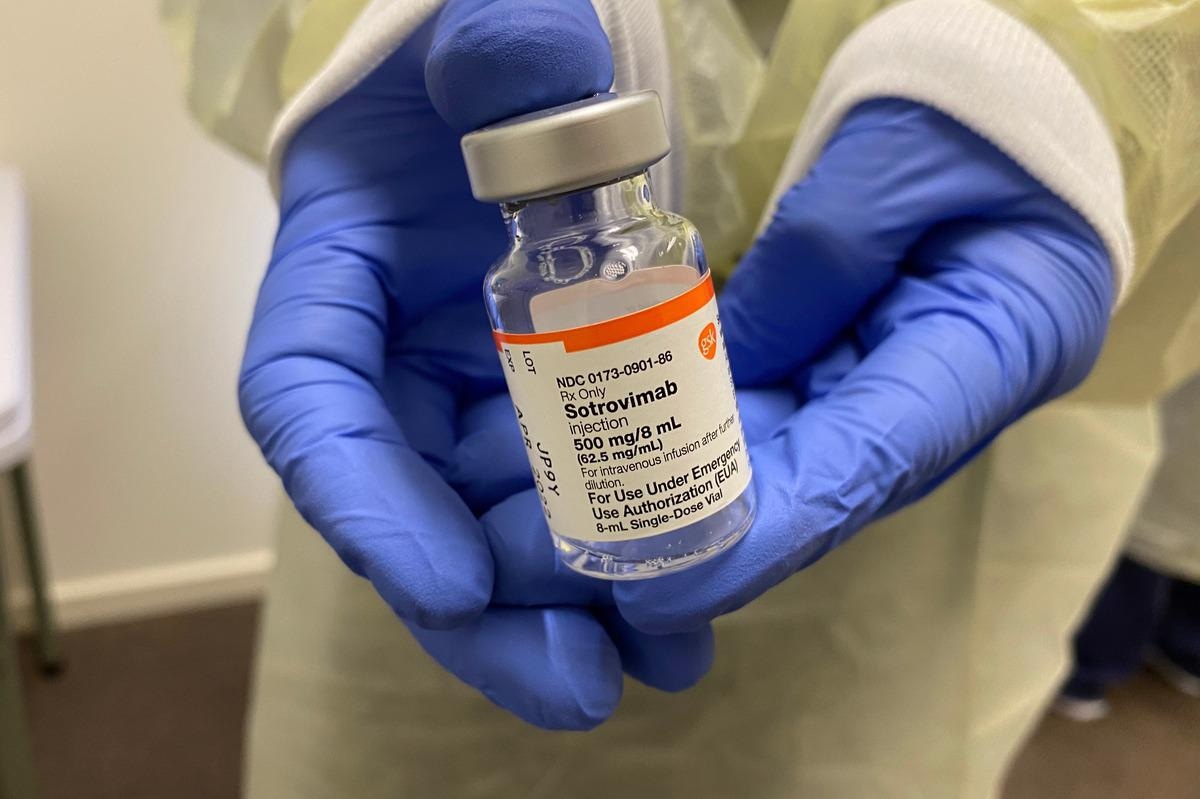
The patient had not received a COVID-19 vaccine and contracted COVID-19 twice. During the first episode of COVID-19 in December 2021, he did not require hospitalization and received an infusion of sotrovimab 500 mg two days after the onset of symptoms, which helped him recover completely.
The patient again contracted COVID-19 in February 2022 and was hospitalized with a high fever, chills, body aches, and severe fatigue. A chest computed tomography (CT) scan showed patchy airspace opacities with consolidation in the left lower lobe of the lung. Although he did not receive antiviral medications, he was prescribed antibiotics for seven days.
Methodology
The researchers confirmed the identity of the SARS-CoV-2 recombinant using four different full-genome sequencing approaches, xGen Amplicon, metagenomics sequencing, AmpliSeq Insight, and ARTIC Amplicon sequencing.
They used VeroE6/transmembrane serine protease 2 (TMPRSS2) cells for viral isolation and seeded them three days before infection to reach 85% to 90% confluency, and checked infected cell monolayers for cytopathic effects (CPE) daily. The team also performed mutation and phylogenetic analysis on SARS-CoV-2 full-genome sequences. Further, they used molecular graphics and homology models for structural analysis of the recombinant S.
Study findings
The study analysis revealed that the entire open reading frame (ORF)1ab genomic region and the beginning of S up to position 22035 contained mutations specific to Delta, closely resembling Delta sublineage AY.45, but no Omicron-specific mutations.
The remaining part of the genome, specifically after position 22193, contained Omicron BA.1-specific mutations and no Delta-specific mutations, indicative of a Delta-Omicron recombination event with a single breakpoint in the 5’ region of the S protein.
Phylogenetic analyses of the distinct subregions corroborated the similarities between the 5’ and 3’ segments with Delta and Omicron lineages, respectively. The re-sequencing results revealed similar 5’ Delta and 3’ Omicron-specific mutations with a breakpoint between base pairs (bp) 22035-22193 in the full-length high-quality sequence.
The metagenomics approach showed an additional Omicron-specific mutation at the beginning of the nine bp insertion at position 22204 (S 214EPE), which was reaffirmed by ARTIC sequencing.
CPE monitoring showed trivial cell rounding in infected monolayers, progressing to all-pervasive cell rounding, debris, detachment, and cell death by 96 hours post-infection (hpi), all suggestive of Omicron. Moreover, recombinant viral cultures did not have typical syncytia formation. Overall, the recombinant virus-induced CPE resembled Omicron closely but not Delta.
Most of the N-terminal domain (NTD) in the recombinant was composed of Delta, while the receptor-binding domain (RBD) and the C-terminal regions of S were of Omicron.
Furthermore, the recombinant SARS-CoV-2 sequence harbored an atypical S mutation (E340D) unrelated to Delta or Omicron which was rarely found in global SARS-CoV-2 sequences. Intriguingly, the E340 mutation was nested in the middle of the sotrovimab binding epitope.
It is worth noting here that the patient received sotrovimab therapy, a class IV anti-S RBD nAb with broad antiviral activity against SARS-CoV-2 when he first contracted COVID-19 in December 2021. The S binding epitope for sotrovimab involves the N-terminus of RBD, and its fragment antigen-binding (Fab) moiety engages the space between RBD and the neighboring NTD.
Conclusions
The recombinant SARS-CoV-2 sequence described in the current study was deposited in the Global Initiative on Sharing Avian Influenza Data (GISAID) database, flagged as a recombinant. It had a single point mutation that split the genome into a 5’ Delta and a 3’ Omicron segment, suggesting that a recombination breakpoint in S NTD is favored, or Omicron’s C-terminal S regions, including RBD, or Delta’s non-structural proteins have selective advantages.
Until now, SARS-CoV-2 recombinants are rare and have not posed a risk of community-level transmission. However, cases similar to the one presented in the current study highlight the need for genomic surveillance to better understand evolutionary leaps that could potentially alter SARS-CoV-2 transmission dynamics, immunity evading potential, or clinical impact.
More importantly, monitoring SARS-CoV-2 infections in immunocompromised populations under treatment with nAbs is also a priority during the ongoing COVID-19 pandemic.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Ralf Duerr, Dacia Dimartino, Christian Marier, Paul Zappile, Guiqing Wang, Jonathan Plitnick, Sara Griesemer, Erica Lasek-Nesselquist, Meike Dittman, Mila Brum Ortigoza, Prithiv J. Prasad, Kirsten St. George, Adriana Heguy. (2022). Delta-Omicron recombinant SARS-CoV-2 in a transplant patient treated with Sotrovimab. bioRxiv. doi: https://doi.org/10.1101/2022.04.06.487325 https://www.biorxiv.org/content/10.1101/2022.04.06.487325v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibody, Antigen, Avian Influenza, Cell, Cell Death, Computed Tomography, Coronavirus, Coronavirus Disease COVID-19, covid-19, CT, Fatigue, Fever, Genome, Genomic, immunity, Influenza, Kidney, Kidney Transplant, Metagenomics, Mutation, Omicron, Pandemic, Point mutation, Prednisone, Protein, Receptor, Renal disease, Respiratory, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sotrovimab, Surgery, Syndrome, Tacrolimus, Tomography, Transplant, Vaccine, Virus

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article
