A new study published in the journal Immunity, by researchers at Trinity College and the University of Manchester has cast new light on how our immune system deals with parasitic worm infection.
The research team focused on a parasitic filarial nematode worm which infects the pleural cavity, the space between the lungs and the chest wall. Despite its clinical relevance, the immunology of the pleural cavity remains remarkably understudied.
According to the World Health Organization, 863 million people are threatened by filariasis, the potentially disfiguring disease caused by the worm. While medical interventions and prevention has been successful in reducing the number of human infections, there are still thought to be more than 70 million people infected each year.
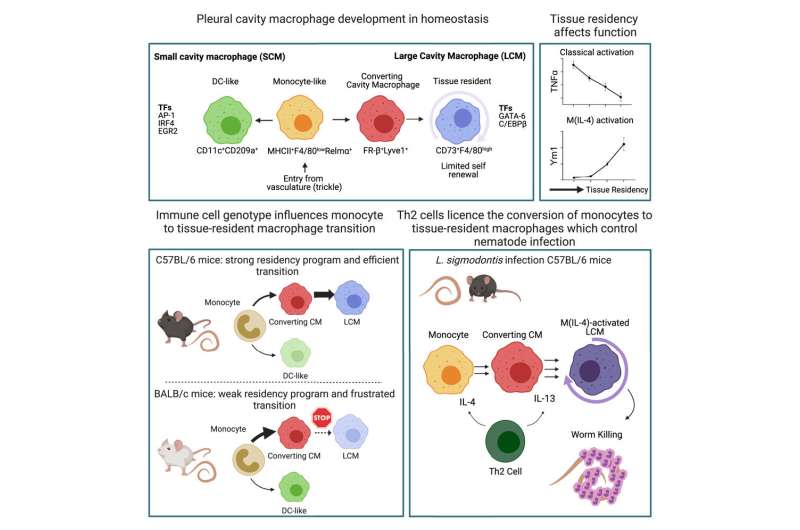
The study shows how a specific type of T-cell (a type of white blood cell), activated by the worms, signal to other immune cells called macrophages to transform and expand in a manner which eliminates the infection by a filarial nematode.
Many people appear to be able to control filarial worm infection while others harbor 100s of worms, some of which go on to develop tissue damage caused by an inappropriate immune reaction to worms. This study is relevant because scientists do not fully understand why some people can handle infection well while others suffer from severe pathology. Compared with worms that live in the gut we have a less clear understanding how the immune system controls infection with filarial nematodes in body tissues.
Dr. Conor Finlay, senior research fellow, Clinical Medicine, School of Medicine, Trinity College and the lead author on the study said, “The signaling molecules or cytokines called IL-4 and IL-13 have long been known to activate macrophages but here we show that they do something surprising, they control the development of blood monocytes into tissue-resident macrophages at the worm infection site. These cytokines are transforming cells into a cell type suitable to fight the worm. What’s more, if we prevent this transformation from occurring then the immune system can no longer kill these worms.”
Furthermore the authors show how T cells—which can generate memory of prior infection—control this whole process, producing the cytokines on macrophages that then go on to kill the worms.
Professor Judi Allen from the Lydia Becker Institute of Immunology and Inflammation at the University of Manchester who supervised the study, said, “For many years my group has tried to understand what role macrophages play during infection of worms that live in the tissues. The finding that they contribute to worm killing is exciting for me personally and opens up even more questions.”
“Tissue-resident macrophages have important roles in controlling inflammation and repairing damaged tissue, so our model of how T cells and cytokines control their development has wide applications in other diseases.”
Dr. Finlay also noted that “this study is not just about worms, we have characterized the immune system of the pleural space to the highest level of detail yet known. Being so close to the lung, the pleural cavity is a site of enormous clinical relevance in congestive heart failure, pneumonia, cancer, and fibrotic diseases. Despite this we know relatively little about the immune response in the pleural space.”
He said that many questions remain unanswered. “We have shown that these macrophages are required for worm killing, now we need to show exactly how they do that. This study leads us to believe that genes which control macrophage function may hold the key to explain the genetic predisposition to infection with parasitic worms.”
More information:
Conor M. Finlay et al, T helper 2 cells control monocyte to tissue-resident macrophage differentiation during nematode infection of the pleural cavity, Immunity (2023). DOI: 10.1016/j.immuni.2023.02.016
Journal information:
Immunity
Source: Read Full Article
