DNA can help to stimulate bone healing in a localized and targeted manner, for example after a complicated fracture or after severe tissue loss following surgery. This has been demonstrated by researchers at Martin Luther University Halle-Wittenberg (MLU), the University of Leipzig, the University of Aveiro (Portugal) and the Fraunhofer Institute for Microstructure of Materials and Systems IMWS in Halle. They have developed a new process in which they coat implant materials with a gene-activated biomaterial that induces stem cells to produce bone tissue. Their findings were published in the journal Advanced Healthcare Materials.
Bones are a fascinating example of the body’s ability to regenerate. They are able to regain full functionality—even after a fracture—thanks to their ability to form new, resilient tissue at the fracture site. “However, when it comes to complicated fractures or major tissue loss, even a bone’s self-healing power is insufficient,” explains Professor Thomas Groth, head of the Biomedical Materials research group at MLU’s Institute of Pharmacy.
“In such cases, implants are needed to stabilize the bone, replace parts of joints, or bridge larger defects with degradable materials.” The success of such implants depends largely on how well they are incorporated into the bone. Increased efforts have been made in recent years to support this process by coating implants with bioactive materials to activate bone cells and mesenchymal stem cells.
Mesenchymal stem cells are capable of generating different types of tissue, however activating them to specifically regenerate bone can be particularly challenging. In such cases, an extracellular matrix plays a crucial role. “The tissue between the bone cells is made up of collagens and chondroitin sulfate, among other things,” explains Groth.
“It can be artificially replicated and applied to the surface of implants to make them bioactive.” This ensures that implants are incorporated better and are less likely to be rejected by the body. Drugs and activators can also be added to the artificial extracellular matrix to stimulate bone growth. One such activator is the protein BMP-2, which is already being used in spinal fusions or to treat complicated, non-healing fractures. However, studies have shown that the high dose of BMP-2 needed can lead to uncontrolled bone tissue formation in the surrounding muscle as well as to other undesirable side effects.
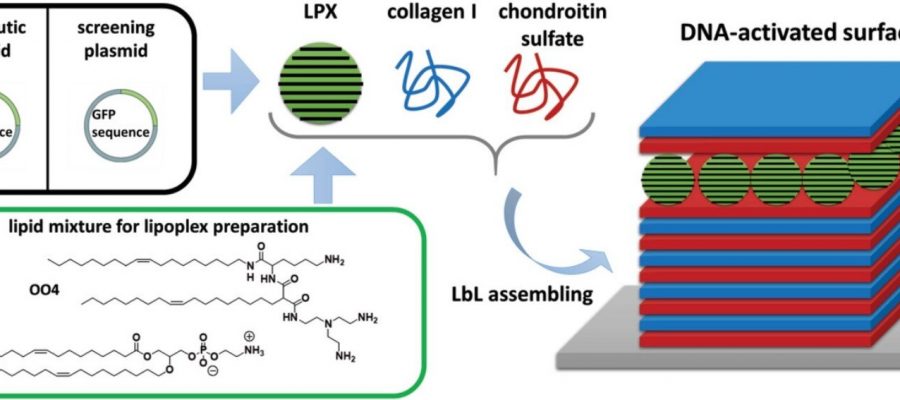
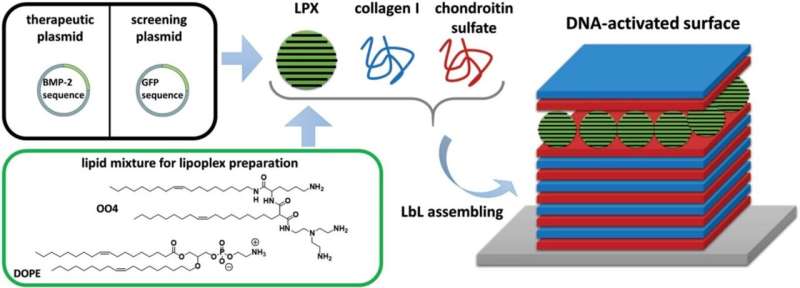
The researchers from Halle, Leipzig and Aveiro are therefore proposing a procedure that stimulates stem cells in a more targeted way and causes significantly fewer side effects. One thing they are focusing on is enhancing the design of the extracellular matrix. They use a special layer-by-layer technology to apply the biomaterial to the implant. This enables them to control its composition, structure and properties at the nano level. “It is a sophisticated process which we have perfected at MLU in collaboration with Fraunhofer IMWS,” explains Thomas Groth.
This design at the nano level is needed to functionalize the biomaterial; here they are leaning on the expertise of colleague Dr. Christian Wölk from Leipzig. Instead of incorporating large amounts of BMP-2 directly into the biofilm and risking an uncontrolled release, he packages DNA fragments into lipid nanoparticles that act as transport containers. Only after the implant has been inserted does the DNA migrate into the cells of the bone tissue and stimulate them to produce BMP-2. This, in turn, activates the bone-forming stem cells.
“Mimicking the extracellular matrix as a thin-film surface coating and functionalizing it with nanoparticles is a milestone in pharmaceutical materials research,” explains Thomas Groth. “DNA can be released in a targeted manner and limits the stimulation of tissue growth with respect to time and location, without causing undesirable side effects.”
According to Groth, the method is also fundamentally suited for transporting mRNA and thus expands the possibilities of regenerative medicine—not only in the field of bone formation, but also for other therapeutic applications.
More information:
Catharina Husteden et al, Lipoplex‐Functionalized Thin‐Film Surface Coating Based on Extracellular Matrix Components as Local Gene Delivery System to Control Osteogenic Stem Cell Differentiation, Advanced Healthcare Materials (2022). DOI: 10.1002/adhm.202201978
Journal information:
Advanced Healthcare Materials
Source: Read Full Article