A team of scientists and doctors from the KK Women’s and Children’s Hospital (KKH), Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) and the Institute for Health Innovation and Technology has discovered a novel, noninvasive method to predict and reduce the relapse of childhood cancers.
The most common form of solid tumor affecting children is neuroblastoma. It is known to be the cause of a disproportionate number of childhood cancer deaths. The majority of relapsed patients would have a very low chance of survival despite being given the best care.
“The bone marrow is the site where majority of neuroblastoma relapses occur. This discovery provides a simplified method of assessing cancer spread. The current method of sampling bone marrow can be complex, painful and costly. This is particularly daunting for young patients and their families,” explained Dr. Amos Loh, Senior Consultant at the Department of Pediatric Surgery, Deputy Chair of the Division of Surgery, and Chair of the Pediatric Brain and Solid Tumor Program, KK Women’s and Children’s Hospital.
“Where current methods may show patients as cancer-free at the end of treatment, our novel approach may detect ‘leftover’ disease not identified by current means. This could one day save patients’ lives through appropriate early interventions to prevent relapse,” added Dr. Loh.
Cancer relapse is usually caused by a small number of “leftover” cancer cells that remain circulating in the blood long after treatment. These cells can eventually settle in various parts of the body and give rise to multiple tumors, years later.
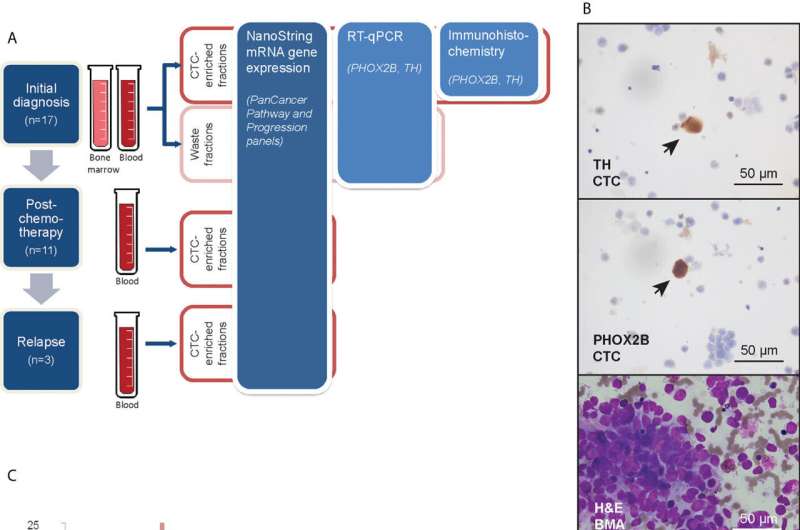
The new, non-invasive method to monitor neuroblastoma is pain-free and less costly, and involves only a small amount of blood from the patient. The blood sample is processed to separate cancer cells from other cells. The cancer cells are then analyzed for genes that would help doctors to determine the likelihood for the cancer to spread to the bone marrow, thereby predicting the likelihood of a relapse. The study identified several genes that predicted relapse in a group of neuroblastoma patients. These include OLFML2B, STAT1, ARHGDIB, STAB1 and TLR2—genes known to be associated with a more aggressive disease state in neuroblastoma.
“We hope that this method can replace current invasive methods such as sampling of bone marrow in the near future, and be potentially expanded to other childhood cancers,” said Associate Professor Chen Zhi Xiong from the Department of Physiology and NUS Centre for Cancer Research at NUS Medicine.
“We are also exploring the use of circulating cancer cells to better understand the biology of neuroblastoma and variations in treatment response to provide more personalized care for neuroblastoma patients. Besides cancer cells, we are also investigating other circulating biological entities in blood that may provide further options to monitor treatment effectiveness, and help predict cancer spread and relapse in childhood cancers.”
The team hopes that the new method of predicting and reducing the relapse of childhood cancers can soon be put to clinical practice in the near future.
Source: Read Full Article
