In a recent study published in Atherosclerosis, researchers investigate the association between non-esterified fatty acids (NEFAs) and incident clinical peripheral artery disease (PAD) in older adults.
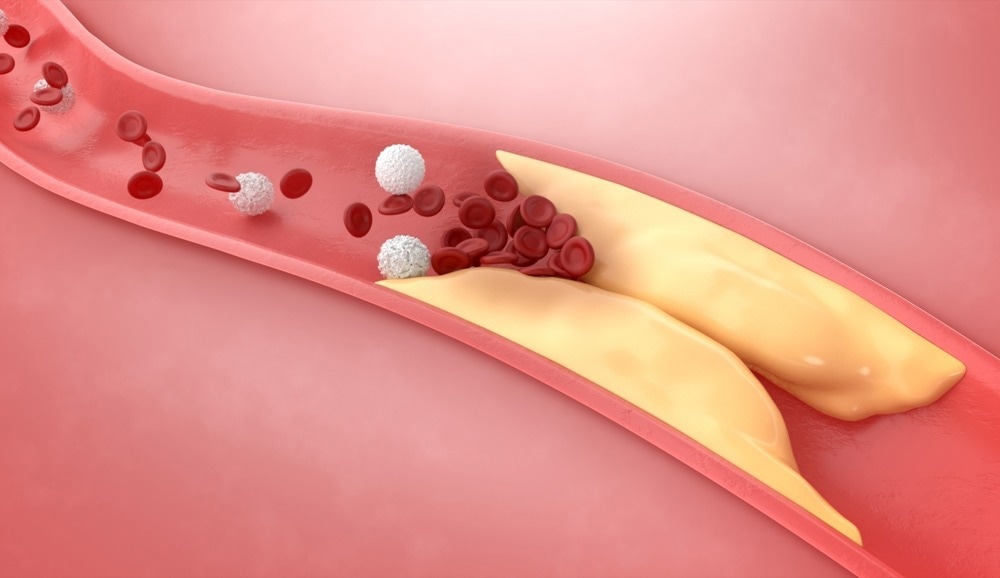 Study: Non-esterified fatty acids and risk of peripheral artery disease in older adults: The cardiovascular health study. Image Credit: NPW-STUDIO/Shutterstock
Study: Non-esterified fatty acids and risk of peripheral artery disease in older adults: The cardiovascular health study. Image Credit: NPW-STUDIO/Shutterstock
How NEFAs may relate to PAD
PAD is a chronic condition resulting from an atherosclerotic obstruction in the arteries of the peripheral vasculature. Previous studies have reported that even a modest decline in the ankle-brachial index (ABI), a measure of PAD severity, is linked to functional impairment.
Circulating NEFAs are associated with disability, frailty, mobility limitations, heart failure, and mortality. Moreover, NEFAs have been linked to endothelial dysfunction, which is a fundamental PAD feature.
NEFA levels in circulation can be modified by pharmacologic interventions. In addition, behavioral factors can help regulate NEFA levels. Therefore, NEFAs can be promising candidates to examine as PAD risk factors.
About the study
The current study evaluated the relationship between NEFAs and incident PAD. Eligible participants were aged 65 or older and not dependent on a wheelchair, institutionalized, or receiving cancer treatment.
A total of 5,201 individuals were recruited into the cardiovascular health study (CHS) between 1989 and 1990. Additional participants were recruited between 1992 and 1993.
Baseline evaluation included questionnaires, anthropometric measurements, physical examination, laboratory investigations, and resting electrocardiography (ECG). Subjects were evaluated every six months between 1989 and 1999, alternating between clinic visits and telephone calls.
The researchers used the 1992-1993 clinic visit as the baseline for the current analysis, as this was when NEFA levels were available for the first time. NEFAs were evaluated in 4,715 participants, 4,575 of whom were examined for incident PAD, as the excluded individuals had prevalent PAD at baseline. Another 184 subjects were excluded from abnormal ABI analysis due to the lack of baseline ABI.
Plasma NEFA concentrations were measured. The researchers also assessed the development of abnormal ABI in those with normal ABI and without PAD at baseline between 1992 and 1993, as well as 1998-1999 examinations.
Cancer Research eBook

Incident clinical PAD risk among those without prevalent PAD was also evaluated at baseline. These results were reported per tertile and standard deviation (SD) increment.
An abnormal ABI was defined as a value of 0.9 or lower with a change of 0.15 or higher. In sensitivity analyses, abnormal ABI was less than or equal to 0.9 or a change of 0.15 or more.
Cox proportional hazards regression was applied to model associations between increments per SD in NEFAs and incident PAD until June 2015. Binary logistic regression was used to model associations between NEFA levels (1992-1993) and abnormal ABI (1998-1999).
Study findings
Older age, female sex, higher body mass index (BMI), hypertension, and diabetes were associated with elevated NEFA concentrations. NEFA levels were associated with an increased risk of incident clinical PAD.
The adjusted hazard ratio for incident clinical PAD was 1.51 and 1.14 per SD increment. Furthermore, an association between NEFAs and an increased risk of abnormal ABI in unadjusted models was observed.
The odds ratio was 0.95 and 1.03 per SD increment for abnormal ABI after statistical adjustment. The results were not different in sensitivity analyses using an alternative definition for abnormal ABI. The correlation between abnormal ABI and incident clinical PAD was not different in a minimally adjusted model.
A significant linear trend was observed for associations between NEFAs and incident clinical PAD, while an insignificant linear trend was observed for abnormal ABI. NEFAs were not associated with incident PAD in the first six years of follow-up but were associated after that period. The hazard ratios within and beyond six years were significantly different, which was also evident in the Kaplan-Meier curve.
Conclusions
Overall, NEFAs showed a significant association with a higher risk of clinical PAD, even after accounting for potential confounders. Meanwhile, no associations were evident with low ABI. The increased risk of PAD associated with NEFAs did not significantly change by race, sex, or fetuin-A, which is a NEFA chaperone protein, levels.
It is not possible to compare the current findings with previous studies, as this study is the first to longitudinally assess associations between NEFAs and PAD. Moreover, these results were only representative of older adults and can not be extrapolated for younger subjects.
Taken together, the study findings indicate that NEFAs may be a promising target for interventions against PAD in the older population.
- Ahiawodzi, P., Solaru, K. W., Chaves, P. H. M., et al. (2023). Non-esterified fatty acids and risk of peripheral artery disease in older adults: The cardiovascular health study. Atherosclerosis. doi:10.1016/j.atherosclerosis.2023.01.020 https://www.atherosclerosis-journal.com/article/S0021-9150(23)00047-3/fulltext
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Atherosclerosis, Body Mass Index, Cancer, Cancer Treatment, Chronic, Diabetes, Disability, Fatty Acids, Heart, Heart Failure, Laboratory, Mortality, Peripheral Artery Disease, Protein, Vasculature, Wheelchair

Written by
Tarun Sai Lomte
Tarun is a writer based in Hyderabad, India. He has a Master’s degree in Biotechnology from the University of Hyderabad and is enthusiastic about scientific research. He enjoys reading research papers and literature reviews and is passionate about writing.
Source: Read Full Article
