When women with rheumatoid arthritis (RA) plan to become pregnant, many anguish over whether to stop their medications, risking a flareup in their disease, or continue with medication and risk possible harm to the baby.
About 50% to 75% will see their disease naturally improve during pregnancy for not-yet-known reasons, while others may see a worsening of their RA. But they have had no way of knowing which would happen to them.
Now, Northwestern Medicine scientists have identified, for the first time, genetic markers that could predict before pregnancy who will improve and who will worsen.
The study, titled “Pre-pregnancy gene expression signatures are associated with subsequent improvement/worsening of rheumatoid arthritis during pregnancy,” was published this week in Arthritis Research & Therapy.
RA is an incurable disease that affects 1% of the adult world population and occurs three times more often among women. It leads to significant disability as a result of inflammation of the joints as well as destruction of cartilage and bone.
“When women with RA go through pregnancy, there often is a natural improvement,” said lead study investigator Damini Jawaheer, research associate professor of medicine in rheumatology at Northwestern University Feinberg School of Medicine. “They describe it as ‘a miracle.’ They say, ‘I have never felt this good with any medication I have taken.’ But the cause of this improvement is a complete mystery.
“If women with RA can know in advance whether they are likely to see their disease disappear during pregnancy, they know they can go off their drugs. Some RA drugs are toxic and affect the fetus, while others are considered safe. But some women with RA don’t want to take any drugs during pregnancy, not even the ones considered safe.”
Being able to predict who will improve and who will worsen will help women in their pregnancy planning and will also help to focus treatment during pregnancy only to those women who are predicted to worsen, Jawaheer said. Furthermore, women who are predicted to improve and their fetus will not be unnecessarily exposed to medications.
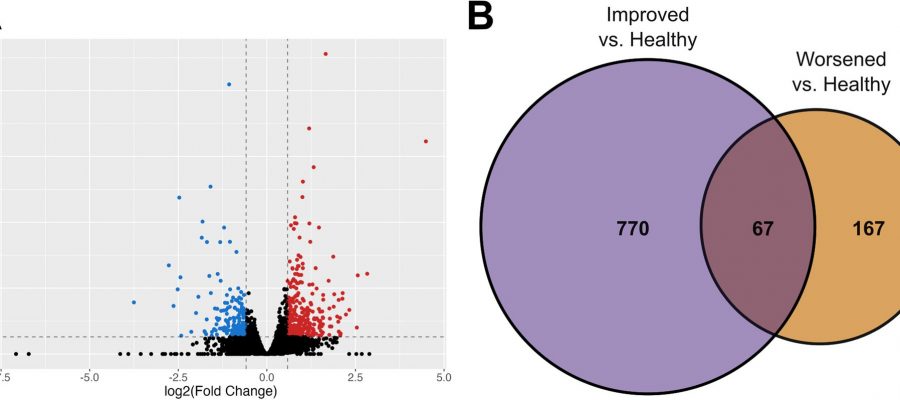
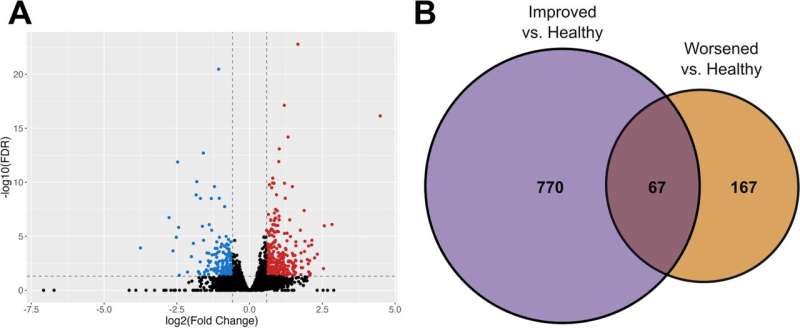
Jawaheer and her team found that before pregnancy, a group of white blood cells called neutrophils were highly expressed among the women who improved during pregnancy, and some genes related to B cells were highly expressed among women who worsened.
This field has not been well studied partly because it is difficult to find women for a pregnancy study before they get pregnant, Jawaheer said.
She and colleagues were able to conduct the study because they’d previously established a unique pregnancy cohort in Denmark, which enrolled women with RA and healthy women before pregnancy and followed them over time to determine who improved and who worsened during pregnancy. Using blood samples collected from those women before pregnancy, they examined the levels of different genes expressed in the blood. Blood samples were collected before pregnancy from 19 women with RA and 13 healthy women enrolled in the prospective pregnancy cohort.
Next, Jawaheer plans to conduct a study in a larger cohort of women to validate these findings. Additionally, her lab is trying to figure out why RA improves during pregnancy.
“How is nature making an incurable disease go away?” she asked. “If we can understand how pregnancy induces a natural improvement, we can use that as a model to develop a new medication that would be safer and could improve the lives of the women and men living with this terrible disease.”
The other Northwestern author is Matthew Wright.
More information:
Matthew Wright et al, Pre-pregnancy gene expression signatures are associated with subsequent improvement/worsening of rheumatoid arthritis during pregnancy, Arthritis Research & Therapy (2023). DOI: 10.1186/s13075-023-03169-6
Journal information:
Arthritis Research & Therapy
Source: Read Full Article