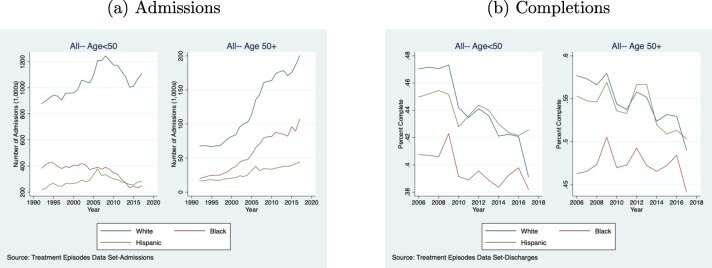
New research co-authored by USC Price visiting scholar Dr. Jevay Grooms in the Journal of Substance Abuse Treatment shows that older Americans are increasingly seeking treatment for substance use disorder (SUD), and there are alarming racial disparities when it comes to completing treatment programs.
Each year between 2006 and 2017, Black Americans over 50 completed treatment programs at a significantly lower rate than white Americans in the same age group. The same was true for Hispanic Americans over 50 with the exception of three years: 2006, 2009 and 2013.
Grooms, an assistant professor at Howard University, published the research alongside Indiana University Assistant Professor Alberto Ortega. Their goal was to examine the economic effects of SUD.
“If you are using substances or you struggle with substance use disorder, chances are you’re not a productive member of society,” Grooms said. “Your ability to work, your ability to hold a job, your ability to provide financially is more limited.”
In their research, Grooms and Ortega used data from the Substance Abuse and Mental Health Services Administration to study SUD admissions, completions and terminations. Grooms noted that a patient can be terminated for a number of reasons, including being asked to leave for not following a facility’s rules or not meeting its expectations. When the pair of researchers broke down their data by race, the results were alarming.
“If you are Black and you enter a treatment facility, you are more likely to be terminated,” Grooms said.
Still, the study’s findings do not fully reflect the realities of everyone with SUD. Many people are underinsured or lack insurance entirely. Grooms says that this is problematic, as the average person seeking treatment goes to a facility twice.
“If you lack health insurance, you may not even go one time—let alone twice,” Grooms said.
There was no clear-cut reason for why older Black subjects had such a low completion rate. However, Grooms has a theory. “We really have a hard time saying with precision what is causing this, but given the history of drugs that have affected inner-city and Black communities, we’re pretty certain that a lot of what’s going on has been influenced by the crack epidemic of the ’80s,” Grooms explained. It’s possible, she shared, that the crack epidemic of the 1980s and early ’90s led to a surge in treatment among people who were in their 20s and 30s, who today fall into the 50-and-older age bracket.
Grooms grew up in Los Angeles and says she witnessed some of the crack cocaine epidemic through extended relatives. “Understanding the way crack has impacted the Black community has always been something that’s [been] with me my whole life,” she said.
Interestingly, Grooms and Ortega found that the completion rates for Black and Hispanic individuals who are younger than 50 are improving, especially in recent years.
In future research, Grooms is interested in evaluating the sub-par policies put in place to fight the crack epidemic—such as over-policing and incarceration—as well as new efforts to reform them.
Said Grooms, “We knew that the way we addressed the crack epidemic was wrong soon after it, but we didn’t think about how to designate funds to help correct it.”
One promising policy change was the implementation of the Affordable Care Act, including the expansion of Medicaid. It is easier to access treatment today than it was in previous decades; and the support is more widely available. Since SUD is now understood as a medical mental health issue, Grooms said, the stigma of “choosing” to have SUD is less pervasive.
In uncovering the rising rate of older Americans seeking care for SUD and the racial disparity that exists in completing treatment, Grooms hopes that two policy objectives will be pursued. The first is boosting public health equity among older adults across racial and ethnic groups.
“People may have implicit biases that they don’t even know are coming into play when making decisions, so if we understand how these implicit biases may impact health outcomes, maybe we can do something to correct them,” Grooms said.
The second is increasing awareness of the financial and social implications of increased SUDs in older populations. Grooms says it is critical to understand the financial vulnerability of older people and the sheer quantity of them; the Census Bureau estimates the number of adults 65 and older will have grown from roughly 40 million in 2010 to 77 million in 2034.
“Going forward, it’s important to think about the way substance use disorder may impact older adults differently today than it did 10 [or] 20 years ago,” Grooms said.
Source: Read Full Article
