Demand for donor livers for transplant patients outstrips supply with over 15% of waitlist patients dying after a year. A new international study offers support for increasing the use of living donor liver transplantation (LDLT) in Western countries and reducing the imbalance between organ supply and demand. This study is reported in the Journal of Hepatology.
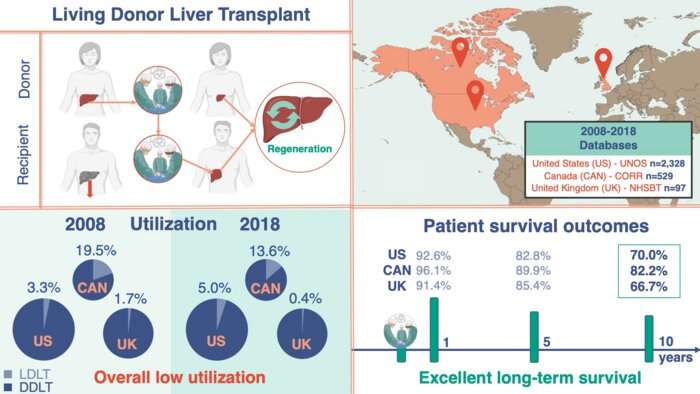
LDLT is when a portion of the liver from a healthy living person is removed and placed into someone whose liver is no longer working properly. The donor’s remaining liver regrows and returns to its normal size, volume, and capacity within a few months after the surgery. Although the waiting period for a deceased donor transplant can be more than five years, LDLT remains uncommon compared to deceased donor liver transplantation (DDLT) in Western countries compared to those in Asia.
Identifying differences in outcomes and other transplant characteristics may help identify areas for healthcare improvement and clarify whether expanding LDLT practices can be justified in countries that rely primarily on DDLT.
“There has been a growing interest in strategies to alleviate the increasing demand for transplantation and the unacceptably high mortality on the liver transplant waitlist,” explained Gonzalo Sapisochin, MD, Ph.D., MSc, Division of General Surgery, University Health Network, Toronto, ON, Canada. “One such approach is LDLT, which can expand the number of grafts available for transplantation. However, short- and long-term outcomes need to be maintained for both the donors and recipients. We therefore sought to compare donor and recipient characteristics and post-transplant outcomes after LDLT.”
This is a retrospective multicenter study of adults aged 18 years or older who underwent primary LDLT between January 2008 and December 2018 as reported by three national liver transplantation registries: United Network for Organ Sharing (UNOS; U.S.), National Health Service Blood and Transplantation (NHSBT; U.K.), and the Canadian Organ Replacement Registry (CORR; Canada). Patients undergoing retransplantation or multi-organ transplantation were excluded. Investigators compared recipient and donor characteristics, temporal trends, and post-LDLT outcomes across the three registries. In addition, they sought to evaluate outcomes for LDLT compared with DDLT within each of the countries.
A total of 2,954 LDLTs were performed in these countries, 2,328 of which took place in the U.S., 529 in Canada, and 97 in the U.K. Canada performed the highest proportion of LDLT procedures over time. Investigators were pleasantly surprised to see that long-term outcomes were excellent despite relatively low use of LDLT in Western countries. The one-, five-, and 10-year patient survival rates were 92.6%, 82.8%, and 70.0% in the U.S.; 96.1%, 89.9%, and 82.2% in Canada; and 91.4%, 85.4%, and 66.7% in the U.K., respectively.
This analysis of LDLT demonstrates that despite the low use of LDLT in Western countries compared to Asian countries, long-term survival is excellent. In addition, the mortality risk is not statistically significantly different between these three countries.
Source: Read Full Article
