Women with high blood pressure during pregnancy had long-term blood pressure and cardiac benefits if their blood pressure was carefully controlled for the first few weeks after having a baby, according to late-breaking science presented today at the American Heart Association’s Scientific Sessions 2023. The meeting, held Nov. 11–13, in Philadelphia, is a premier global exchange of the latest scientific advancements, research and evidence-based clinical practice updates in cardiovascular science. The full manuscript is also simultaneously published Nov. 11 in JAMA.
“The heart undergoes significant changes during any pregnancy to cope with the increased circulatory demands of the growing baby, and these changes are much more profound during a hypertensive pregnancy, because of the increased stress of the pregnancy,” said lead study author Paul Leeson, M.B., B.Chir., Ph.D., a professor of cardiovascular medicine at the University of Oxford in the United Kingdom.
“Women who have had uncontrolled high blood pressure during pregnancy are at significantly greater risk of complications with their heart longer term. One-third develop hypertension again within 10 years of pregnancy and their risk of early heart attack and stroke are doubled.”
In this prospective, randomized trial conducted in the U.K., researchers investigated the effects of improving blood pressure control immediately after pregnancy on long-term blood pressure levels.
This study included 220 new mothers who had high blood pressure during pregnancy and still needed medication for high blood pressure after giving birth.
Half of the participants were randomly assigned to the group that received a wireless blood pressure monitor and asked to send daily blood pressure readings via a phone app to the study doctors. The phone and app were connected to the blood pressure monitor via Bluetooth, and blood pressure measures were automatically uploaded to the app and automatically shared with the study doctors. The app sent automated prompts to the participants based on their blood pressure levels—to either repeat a reading or, if the reading was in a range that needed changes to their blood pressure medication, advised them to contact their doctor in the trial. The doctors then advised participants via phone or video call about how to adjust their medication to make sure their blood pressure remained below 140/90 mm Hg.
The remaining half of the participants received usual postpartum care, which, in the U.K., involves an office visit with the family physician or midwife 5–10 days after delivery and another at 6–8 weeks after giving birth.
“The trial suggests the timing of this second appointment may miss a critical window for early blood pressure optimization,” Leeson said. “While this visit includes a blood pressure examination and participants are likely to be on blood pressure medication until their blood pressure is back in a normal range, their blood pressure will not be as carefully monitored and medication will not be as tightly adjusted as in the intervention group of the trial.”
The trial results found:
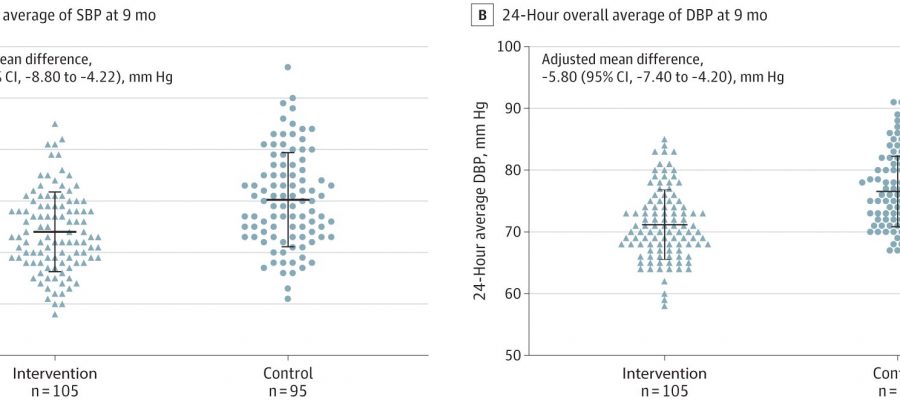
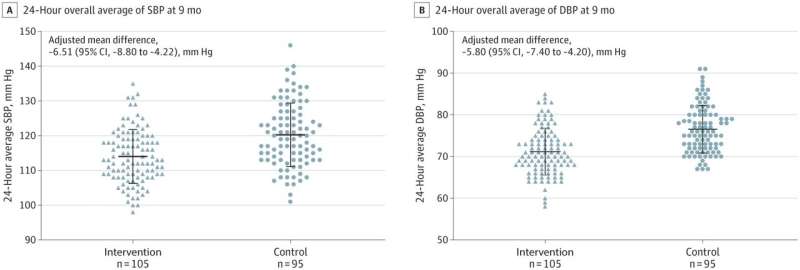
- Nine months after delivery, the women in the intervention group had an average clinic blood pressure of 126/82 mm Hg, compared to 131/86 mm Hg for the women who received usual care.
- This long-term reduction in blood pressure was seen even though 70% of the women in both groups no longer needed high blood pressure medication by around six weeks after delivery. Participants in the intervention group had a median duration of treatment with anti-hypertensive medication of 39 days.
- The effect on lowering high blood pressure persisted for eight to nine months after participants stopped taking high blood pressure medication.
- Fewer women who received the intervention needed to go back into the hospital in the first three weeks after delivery as a result of high blood pressure.
“We were surprised by the size and consistency of the blood pressure reduction in the women who received the intervention. The benefits started to emerge within the first week or two after pregnancy, and the effect on blood pressure persisted after the medication was stopped,” Leeson said.
“A 5–10 mm Hg reduction in blood pressure is typically associated with a 20% reduction in longer-term cardiovascular risk,” he added. “If the reduction in blood pressure we observed at nine months is sustained long-term, this could slow progression to needing treatment for hypertension by an average of up to a decade.”
Approximately 90% of participants agreed to have the researchers also perform cardiac magnetic resonance imaging and echocardiography on them at nine months postpartum. Women who had received the tighter blood pressure control after delivery showed clear improvements in the structure and function of the heart compared to women who had usual care.
Study details and background:
- Approximately 80% of the participants were white women, with an average age of 33 years.
- Approximately 65% of the study participants had just completed their 1st pregnancy, 30% had completed their second pregnancy and 5% had completed their 3rd pregnancy.
Study limitations included that the study was conducted at a single research center, meaning that the intervention may need to be modified before being repeated at multiple centers, and that the research team delivering the study intervention knew who had the self-monitoring devices, which may bias results. To overcome this potential for bias, the researchers ensured that blood pressure measurements were digitally collected by the participants’ 24-hour blood pressure machines, which downloaded measurements and added them to the research database. This method was independent of the study team and mothers, and those who conducted the analysis were blinded to how the home blood pressure monitoring devices were allocated, Leeson said.
Future work will involve replicating the study in more racially and ethnically diverse patient populations in the U.K., identifying the optimal way to provide care after pregnancy and exploring the potential mechanisms of cardiac remodeling that may underpin the long-term lowering of blood pressure, Leeson said.
The 2017 ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults classifies stage 1 hypertension as having clinic top and bottom numbers greater than or equal to 130/80 mm Hg and stage 2 hypertension as having top and bottom numbers greater than or equal to 140/90 mm Hg.
More information:
Jamie Kitt et al, Long-Term Blood Pressure Control After Hypertensive Pregnancy Following Physician-Optimized Self-Management, JAMA (2023). DOI: 10.1001/jama.2023.21523
Journal information:
Journal of the American Medical Association
Source: Read Full Article