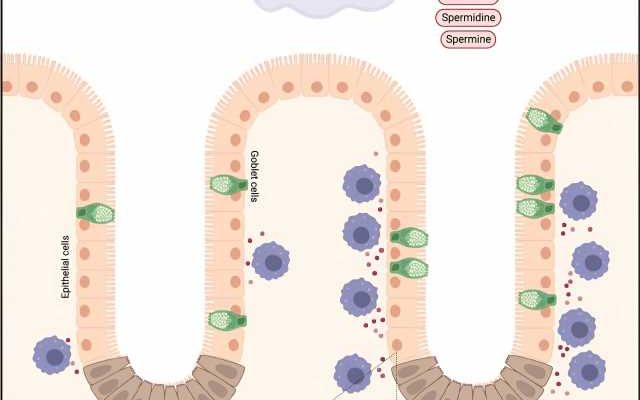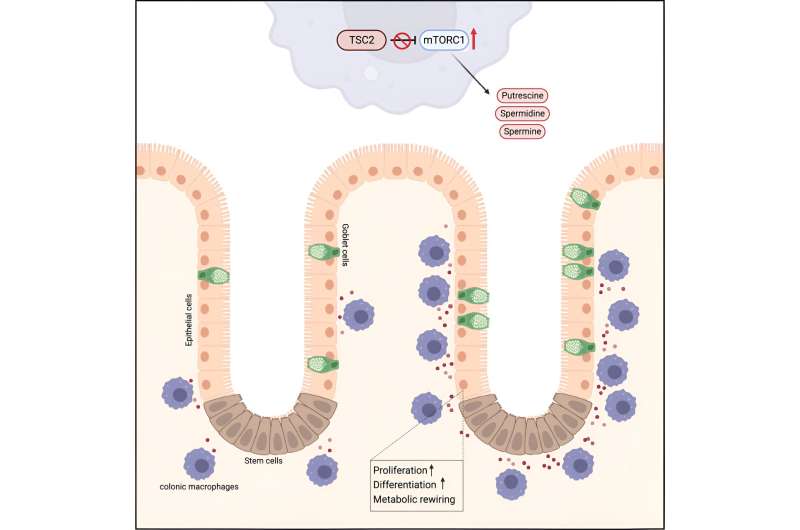
A research team from MedUni Vienna has now demonstrated for the first time the central role of macrophages in the renewal of intestinal cells, which sheds light on the complex interplay between immune cells and tissue regeneration. In particular, it could be described that macrophages produce the metabolites spermidine and spermine in high amounts, which then benefit the other tissue cells in the organ.
As a result, the tissue cells no longer need to produce these substances themselves and are better able to perform their proper functions. This first description of a “commensal metabolism” of macrophages was recently published in the journal Cell Metabolism.
The intestine, which is responsible for digesting food and absorbing nutrients, relies on a single layer of epithelial cells (surface cells) to maintain the integrity of the intestinal barrier. These cells are completely renewed every four to seven days. This process is critical to protecting the body from microbial threats, maintaining intestinal function, and preventing diseases such as inflammatory bowel disease and colon cancer.
Macrophages are immune cells that are found in every organ of the body. The research team, led by Thomas Weichhart of MedUni Vienna’s Center for Pathobiochemistry and Genetics and coordinator of the SFB Immunometabolism, discovered that macrophages in the colon are strategically positioned in close proximity to intestinal epithelial cells.
The researchers identified a crucial mechanism by which these macrophages support the proliferation of epithelial cells. This metabolic support was particularly important during periods of proliferative stress, such as inflammation-related colitis.
First author of the study Stephanie Fritsch comments, “We were able to show that macrophages produce large amounts of the polyamines spermidine and spermine via the mTORC1 signaling pathway”. These polyamines were taken up by the epithelial cells, leading to a switch in their cell metabolism, promoting their proliferation and strengthening their defense mechanisms.
Spermine in particular had a major stimulatory effect on the proliferation of colon cells. Importantly, this mTORC1 activation and polyamine production had a protective effect against inflammatory bowel injury in animal models. Polyamines especially spermidine have been heavily researched for some time as studies show that these substances can prolong life and slow down the aging process.
Macrophages support the metabolism of other cells
This research represents a paradigm shift in understanding the gut microenvironment. It highlights macrophages for the first time as “metabolic factories” that support the metabolism of other cells, which is critical for efficient self-renewal of the intestinal epithelium.
In addition, the study offers insights into potential therapeutic targets for inflammatory bowel disease and other disorders related to gut dysfunction.
Paving the way for new therapies for tissue regeneration and intestinal diseases
Thomas Weichhart says, “Thanks to the support of the FWF within the framework of this special research area, these findings have become possible.” SFB F83 Immunometabolism includes groups from Vienna and Graz that are investigating the metabolic interaction of tissue cells and macrophages. The results of this study open promising avenues for future research.
Researchers may investigate the manipulation of macrophage-mediated metabolic support as a strategy to enhance tissue regeneration and combat intestinal diseases. In addition, further investigation of the role of polyamines and mTORC1 signaling in immune cells may reveal new therapeutic approaches.
“The results represent a significant step forward in our quest to better understand the gut and improve human health,” said Thomas Weichhart.
More information:
Stephanie Deborah Fritsch et al, Metabolic support by macrophages sustains colonic epithelial homeostasis, Cell Metabolism (2023). DOI: 10.1016/j.cmet.2023.09.010
Journal information:
Cell Metabolism
Source: Read Full Article