When the new SARS-CoV-2 virus began killing thousands of people every week, physicians and scientists around the globe raced to learn why the new pathogen was so deadly. Among many early findings, experts noted that the infection played havoc with blood circulation, both inflaming the linings of blood vessels and making the blood itself more likely to form dangerous clots.
Critically ill COVID-19 patients suffered pulmonary embolisms, deep vein thrombosis (DVT), arterial thrombosis, as well as microvascular thrombosis affecting tissues of the lungs, kidneys, and heart.
Doctors tried a wide array of existing medications in hopes of controlling the blood system impacts, with mixed results at best. Especially early on, care teams were flying blind. Vital information about the cellular mechanisms affected by the virus remained largely unknown.
Frustrating the search for effective treatments, the traditional research approach based on studying data from mouse models was not generating useful answers. Mice simply do not experience infections from this virus the same ways people do. Nor do other rodents.
Enter the emerging field of organoid medicine.
Lab-grown human tissues demonstrate value
In the past two decades, scientists have made impressive strides at coaxing human stem cells to form tiny-but-functional versions of human organs. Cincinnati Children’s has been a leader in this field, with groundbreaking developments of tissues that mimic the functions of the intestine, stomach, esophagus and more.
Now, an expert at Cincinnati Children’s working with a team of colleagues in Japan has applied organoid technology to make a significant discovery in the race to develop effective COVID treatments. Their findings were published online Oct. 5, 2023, in the journal Cell Stem Cell.
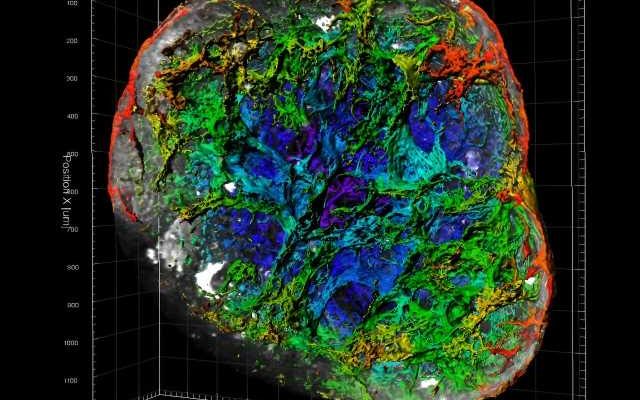
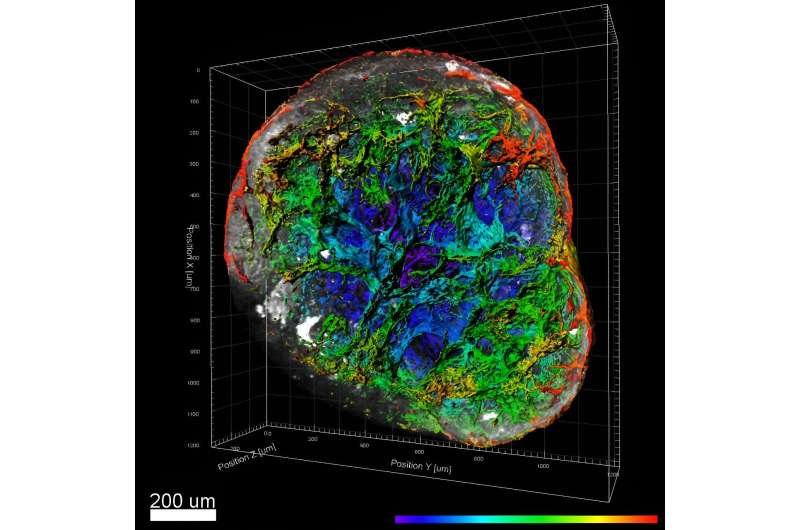
“We developed a human vascular organoid model that accurately mimics the damage caused by SARS-CoV-2,” says the study’s corresponding author Takanori Takebe, M.D., Ph.D. “After conducting many proteomic, genetic and other studies, we determined that the severe vascular damage and thrombosis associated with COVID-19 can be mitigated by a long-acting monoclonal antibody that targets the complement amplification cycle regulated by factor D (CFD).”
Takebe is an expert in organoid medicine who holds dual appointments with Cincinnati Children’s and Tokyo Medical and Dental University. He also serves as director for commercial innovation at Cincinnati Children’s Center for Stem Cell and Organoid Research and Medicine (CuSTOM). Co-first authors of the study were Eri Kawakami, Ph.D., with the Takeda Pharmaceutical Company, and Norikazu Saiki, Ph.D., at Tokyo Medical and Dental University.
Next steps: Build on modest initial benefits
In addition to the organoid tissue findings, the research team confirmed many of their observations with testing involving macaque monkeys. All of the primate studies were conducted in Japan.
The team reports, however, that the particular monoclonal antibody used in the study resulted in only modest reductions in inflammation. Next steps include further testing involving “humanized” animal models to accurately assess the impact of a clinical-grade CFD targeted antibody, Takebe says.
More information:
Complement factor D targeting protects endotheliopathy in organoid and monkey models of COVID-19, Cell Stem Cell (2023). DOI: 10.1016/j.stem.2023.09.001. www.cell.com/cell-stem-cell/fu … 1934-5909(23)00322-3
Journal information:
Cell Stem Cell
Source: Read Full Article