When non-invasive sound waves break apart tumors, they trigger an immune response in mice. By breaking down the cell wall “cloak,” the treatment exposes cancer cell markers that had previously been hidden from the body’s defenses, researchers at the University of Michigan have shown.
The technique developed at Michigan, known as histotripsy, offers a two-prong approach to attacking cancers: the physical destruction of tumors via sound waves and the kickstarting of the body’s immune response. It could potentially offer medical professionals a treatment option for patients without the harmful side effects of radiation and chemotherapy.
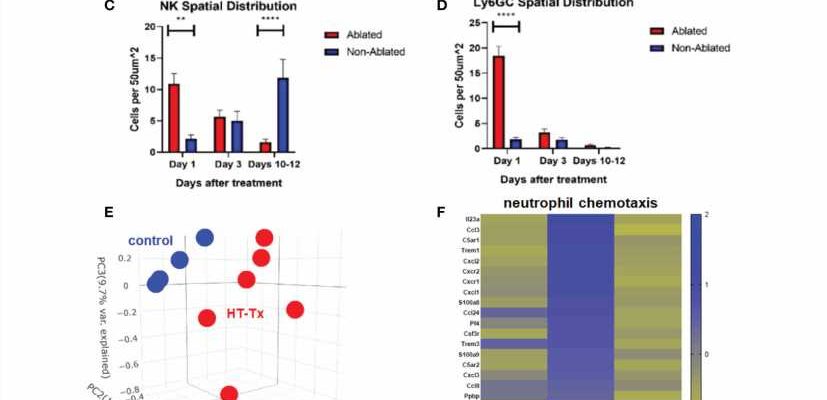
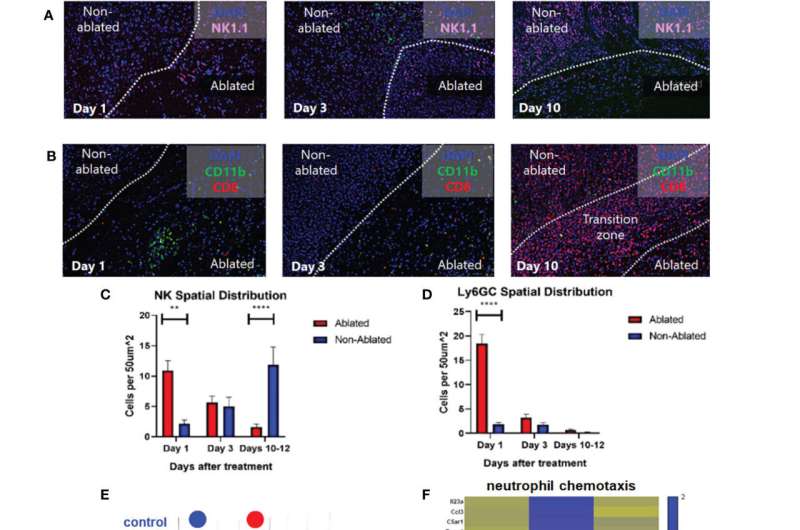
Until now, researchers didn’t understand how histotripsy activated the immune system. A study from last spring showed that histotripsy breaks down liver tumors in rats, leading to the complete disappearance of the tumor even when sound waves are applied to only 50% to 75% of the mass. The immune response also prevented further spread, with no evidence of recurrence or metastases in more than 80% of the animals.
“We found that histotripsy somehow not only kills cancer cells, but causes them to undergo a unique pathway of cell death that draws the attention of the immune system,” said Clifford Cho, the C. Gardner Child Professor of Surgery and vice chair of surgery, whose lab designed immune study protocols and measured immune responses for the study published this month in Frontiers in Immunology.
The key turned out to be tumor antigens—proteins only found in cancer cells and hidden behind their cell walls. When cells die by chemotherapy or radiation, these antigens are destroyed in the process. In contrast, sound waves kill the cancer cells by breaking their cell walls, releasing tumor antigens that then trigger the body’s defense systems.
The immune response occurred throughout the body, not simply in the area where the histotripsy was applied.
“With histotripsy, we’re not destroying the antigens, we’re releasing them while killing the tumor cells,” said Zhen Xu, U-M professor of biomedical engineering and an inventor of the histotripsy approach. “Once they’re no longer hidden, the body can see them and attack them.”
The team was able to discover the mechanism due to the way mice in cancer studies are typically given genetically identical tumors. After breaking up a tumor in one mouse using histotripsy, the team extracted some of that material, homogenized it and injected it into another mouse. Both mice developed immune protection from that cancer.
“Injecting the debris into a second mouse had almost a vaccine-like property,” Xu said. “Mice that received this debris were surprisingly resistant to the growth of cancers.”
Since 2001, Xu’s laboratory at the University of Michigan has pioneered the use of histotripsy in the fight against cancer, leading to the multi-center clinical trial #HOPE4LIVER. More recently, the group’s research has produced promising results on histotripsy treatment of brain cancer therapy and immunotherapy.
More information:
Ashley L. Pepple et al, Spatiotemporal local and abscopal cell death and immune responses to histotripsy focused ultrasound tumor ablation, Frontiers in Immunology (2023). DOI: 10.3389/fimmu.2023.1012799
Journal information:
Frontiers in Immunology
Source: Read Full Article