Substantial variation in infectiousness among cases may strongly impact the way SARS-CoV-2 virus spreads in the population, even at the household level, shows a study published March 7 in eLife.
The findings may help epidemiologists better understand the role of individual differences in infectiousness in the spread of SARS-CoV-2. Understanding these patterns will help public health teams develop more effective ways to reduce transmission.
The role of so-called “superspreading events” in transmitting SARS-CoV-2 has been well studied during the COVID-19 pandemic. Many studies have focused on group events that led to numerous infections. The overall results suggest that 20% of infected individuals cause 80% of virus transmission, but it is unclear if such transmission heterogeneity is driven by the difference in the number of exposed contacts rather than biological and behavioral factors.
“The risk of SARS-CoV-2 transmission at home is four to ten times higher than in other places,” says lead author Tim Tsang, Assistant Professor in the Division of Epidemiology and Biostatistics at the University of Hong Kong School of Public Health in Pokfulam. “Studying home transmission where the numbers of exposed individuals are easier to track may give us more accurate estimates of individual variation in infectiousness.”
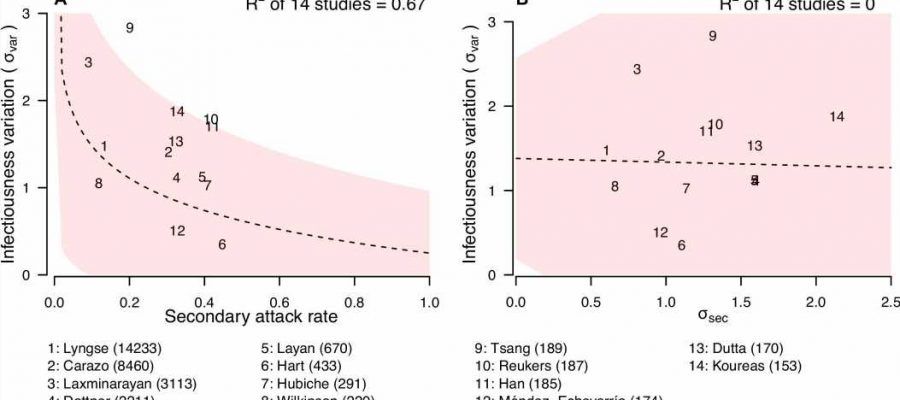
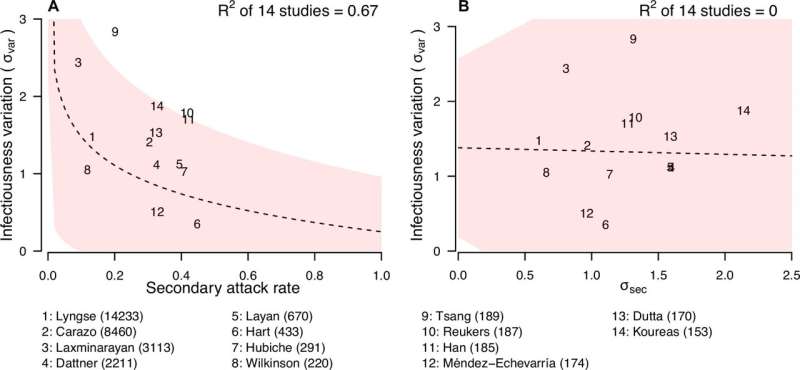
Tsang and colleagues analyzed data from 17 studies of household transmission of SARS-CoV-2, conducted early in the pandemic when the original strains were circulating. The analysis included 13,098 COVID-19 index cases—some of the first cases where patients were diagnosed with the virus—and 31,359 household contacts.
The team used the data to create a mathematical model that describes the differences in the number of household contacts infected by each individual with COVID-19. The model showed that the top 20% most infectious people caused three times more infections among household contacts than the average person with COVID-19.
Subsets of individual superspreaders were even more infectious, the model shows. About 6% of individuals infected about eight times more people, and about 15% infected about four times more.
“There is substantial variation in individual infectiousness within households,” says co-senior author Simon Cauchemez, head of the Mathematical Modeling of Infectious Diseases Unit at the Institut Pasteur, Université Paris Cité, France. “These differences may be caused by individual biology, behavior, or demographic factors.”
For example, adults with COVID-19 may be more likely than young children to self-isolate or engage in behaviors such as mask-wearing that may reduce transmission to others in their household. Factors such as household wealth may have also determined whether individuals had access to masks or separate bathrooms during infection.
However, the team did not have access to data on individual characteristics, for example age or gender, or demographic data such as household income. They also did not look at index patient symptoms, or factors including whether household contacts had characteristics or conditions that made them more vulnerable to infection.
Despite these limitations, the study demonstrates a high level of variation in individual infectiousness in the home setting and provides a modeling tool for future investigations of variability in infectiousness.
“Our tool will provide a new way for epidemiologists to measure individual differences in infectiousness in household settings,” says co-senior author Benjamin Cowling, Professor at the World Health Organization Collaborating Center for Infectious Disease Epidemiology and Control at the University of Hong Kong School of Public Health. “We hope this information will help public health officials craft improved methods for curbing the spread of SARS-CoV-2 or other infectious diseases.”
More information:
Tim K Tsang et al, The effect of variation of individual infectiousness on SARS-CoV-2 transmission in households, eLife (2023). DOI: 10.7554/eLife.82611
Journal information:
eLife
Source: Read Full Article