
Hospital-acquired COVID-19 mortality drops in Omicron era post-vaccination, reveals Swedish study
In a retrospective, matched cohort study published in JAMA Network Open, researchers investigated the incidence of hospital-acquired (nosocomial) severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and the related 30-day mortality among patients hospitalized in Stockholm, Sweden. They found that nosocomial SARS-CoV-2 infections in the pre-vaccination period and the initial days of the coronavirus disease 2019 (COVID-19) pandemic were associated with an increased 30-day mortality. In contrast, they found a lower 30-day mortality in the post-vaccination phase during the Omega variant wave.
 Study: Nosocomial SARS-CoV-2 Infections and Mortality During Unique COVID-19 Epidemic Waves. Image Credit: Ground Picture / Shutterstock
Study: Nosocomial SARS-CoV-2 Infections and Mortality During Unique COVID-19 Epidemic Waves. Image Credit: Ground Picture / Shutterstock
Background
Nosocomial SARS-CoV-2 infections are reported to be associated with a 1.3-fold higher mortality risk as compared to community-acquired SARS-CoV-2 infections. Additionally, hospitalized patients are more likely to acquire a SARS-CoV-2 infection. As most of the previous studies in the field focus on patients admitted to the hospital with community-acquired SARS-CoV-2 infection, the excess mortality due to severe SARS-CoV-2 infections among hospitalized patients remains to be investigated, especially during the Omicron wave of the pandemic. Therefore, researchers in this study aimed to study the incidence of hospital-acquired SARS-CoV-2 infections and the associated mortality of patients and examined the potential effect of vaccination on mortality in the pre-and post-vaccination era of the pandemic. The objective of the study was to evaluate the need for measures for infection prevention and control (IPC).
About the study
The present observational cohort study was conducted retrospectively and included 303,898 individuals aged 18 years and above who were hospitalized in Region Stockholm hospitals between March 2020 and September 2022. The entire duration of the study was divided into three phases: the "pre-vaccination" period (March 1, 2020, to January 24, 2021), the post-vaccination "period 1" (January 25, 2021 to January 6, 2022), the post-vaccination "period 2" (January 7, 2022 to September 15, 2022). The Omicron variant predominated the SARS-CoV-2 infections in the post-vaccination period 2.
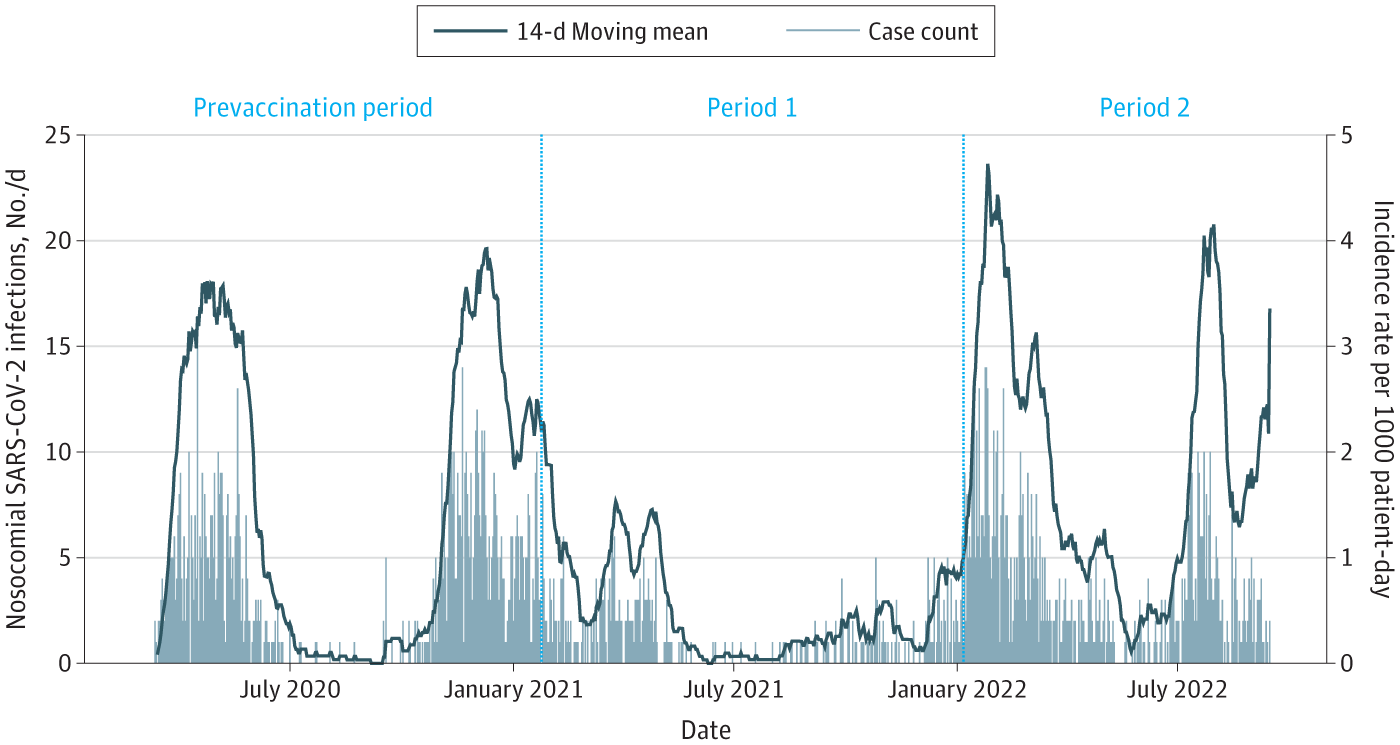
The left axis shows the daily count of nosocomial SARS-CoV-2 infections between March 2020 and September 2022. The right axis shows the incidence rate of nosocomial SARS-CoV-2 infections between March 2020 and September 2022 calculated using a 14-day moving mean. To calculate the patient-days at risk, only admissions with length of stay greater than 7 days were included.
Data regarding the included patients' hospital admission, demographics, and comorbidities were retrieved from the Region Stockholm Data Warehouse. Information on the positive results of the SARS-CoV-2 polymerase chain reaction (PCR) tests was obtained from SmiNet, while information on the negative test results was obtained from the Quality Register for SARS-CoV-2 and electronic health records. A SARS-CoV-2 infection was determined as nosocomial, community-acquired, or indeterminate using specific criteria designed based on the day of the PCR test, the number of days post-hospitalization, the number of days post-discharge, and the length of the stay. A SARS-CoV-2 infection was termed as nosocomial if the first positive PCR test result was obtained at least eight days post-hospitalization or within two days post-discharge. Further, the index date was determined for each patient.
Patient admissions with nosocomial SARS-CoV-2 infections ("COVID-19 admissions") were matched with those without SARS-CoV-2 infections ("non-COVID-19 admissions"). While the primary outcome was 30-day mortality from the index date, the secondary outcomes were 31–90-day mortality and the number of hospital-free days (HFDs). The statistical analysis included the use of adjusted hazard ratio (AHR), Kaplan-Meier curves, Cox proportional hazards regression models, moving means, and sensitivity analyses, among other tools.
Results and discussion
During the entire duration of the study, nosocomial SARS-CoV-2 infections were identified in 2193 individuals of median age 80 years, with 50.5% being female participants. While the overall incidence rate was found to be 1.57 per 1000 patient days, it was found to be 1.79. 0.94 and 2.25 in the pre-vaccination phase and post-vaccination periods 1 and 2, respectively.
The outcomes of nosocomial COVID-19 hospitalizations (n=1487) were matched with non-COVID-19 hospitalizations (n=5044). The cumulative 30-day mortality was found to be lower in non-COVID-19 admissions (11%, n = 4872) than in COVID-19 admissions (25%, n = 1452). The 30-day mortality was found to be higher in the pre-vaccination period (AHR = 2.97) as compared to period 1 (AHR = 2.08) and period 2 (AHR = 1.22). Among COVID-19 admissions, the 30-day mortality was found to be lower (AHR = 0.64) in those ≥2 doses of SARS-CoV-2 vaccination as compared to those with less than two doses, indicating 40% protection offered by two-dose vaccination. Further, in the COVID-19 admissions group, the median HFD increased from 6 in the pre-vaccination phase to 13 and 19 in periods 1 and 2, respectively. In contrast, HFD remained constant for the non-COVID-19 group throughout the three phases of the study.
Although the study is strengthened by its generalizability (owing to the use of complete data), it is limited by the lack of availability of extensive community testing in parts of the study (before June 2020 and after February 2022) and the smaller sample size.
Conclusion
Taken together, the results of this study provide valuable insights into the burden of nosocomial SARS-CoV-2 infections in Stockholm while shedding light on the potential influence of successful vaccination and the emergence of less severe variants of the virus on excess mortality risk. The findings suggest that IPC measures are crucial to reducing the risk of excess mortality and nosocomial transmission, especially when the population immunity is low. Further research is needed to understand the association between nosocomial infections and mortality in high-risk groups and the effect of booster vaccination on public health outcomes.
- Nosocomial SARS-CoV-2 infections and mortality during unique COVID-19 epidemic waves. Dave N et al., JAMA Network Open, 6(11):e2341936 (2023), DOI: 10.1001/jamanetworkopen.2023.41936, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2811647
Posted in: Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Coronavirus, Coronavirus Disease COVID-19, Hospital, immunity, Mortality, Omicron, Pandemic, Polymerase, Polymerase Chain Reaction, Public Health, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus

Written by
Dr. Sushama R. Chaphalkar
Dr. Sushama R. Chaphalkar is a senior researcher and academician based in Pune, India. She holds a PhD in Microbiology and comes with vast experience in research and education in Biotechnology. In her illustrious career spanning three decades and a half, she held prominent leadership positions in academia and industry. As the Founder-Director of a renowned Biotechnology institute, she worked extensively on high-end research projects of industrial significance, fostering a stronger bond between industry and academia.