
Halting pandemics at the source: The call for a proactive 'One Health' approach
In a recent review published in the journal PLoS Pathogens, a group of authors prioritized the primary prevention of pathogen spillover, integrated a One Health approach, and harnessed global initiatives and investments for a comprehensive strategy to avert future pandemics at their source.
 Opinion: Prevention of zoonotic spillover: From relying on response to reducing the risk at source. Image Credit: Maximillian cabinet / Shutterstock
Opinion: Prevention of zoonotic spillover: From relying on response to reducing the risk at source. Image Credit: Maximillian cabinet / Shutterstock
Background
The coronavirus disease 2019 (COVID-19) pandemic's global health toll has intensified discussions on better pandemic preparedness. A major cause of emerging infectious diseases is the zoonotic spillover from animals to humans, influenced by factors like deforestation and agricultural shifts. Despite the evident economic benefits of prevention, many strategies, like the World Bank Pandemic Fund, primarily emphasize reaction over proactive prevention. The "prevention paradox " may influence such a stance," overlooking the substantial economic and societal returns from preemptive actions. Notably, while significant investments are made in areas like counter-terrorism or flood management to mitigate potential risks, a similar emphasis on pandemic prevention remains elusive. Further research is needed to ascertain the optimal resource allocation for proactive pandemic prevention, emphasizing the mitigation of zoonotic spillover drivers to shift from costly reactive strategies to more sustainable preventive ones.
Understanding "prevention of spillover"
Contextualizing "prevention" in health settings
To ensure that actions and resources are aptly directed, it is crucial to clearly define "prevention of spillover" concerning outbreaks, disease endemicity, epidemics, and pandemics. Currently, the interpretation of "prevention" varies based on context. In public health, for instance, it might denote the complete avoidance of human disease (primary prevention) or inhibiting localized disease outbreaks from escalating into more significant crises (secondary prevention). Secondary prevention encompasses methods like vaccination, early detection, enhancement of health systems, health advocacy, drug therapy, behavior modification, and sanitation. However, to mitigate misunderstandings, secondary prevention might be better labeled as "containment of infection" since it aptly conveys its purpose in contrast to the prevention of spillover.
For the purposes of this discussion, "prevention of spillover" is about hindering that initial and crucial step: halting pathogens from moving from animals to humans. Although our focus here is predominantly on human pandemic prevention, it is vital to acknowledge that human actions facilitating spillover between various species (like through the wildlife trade) can also wreak havoc on wild and domesticated animal populations.
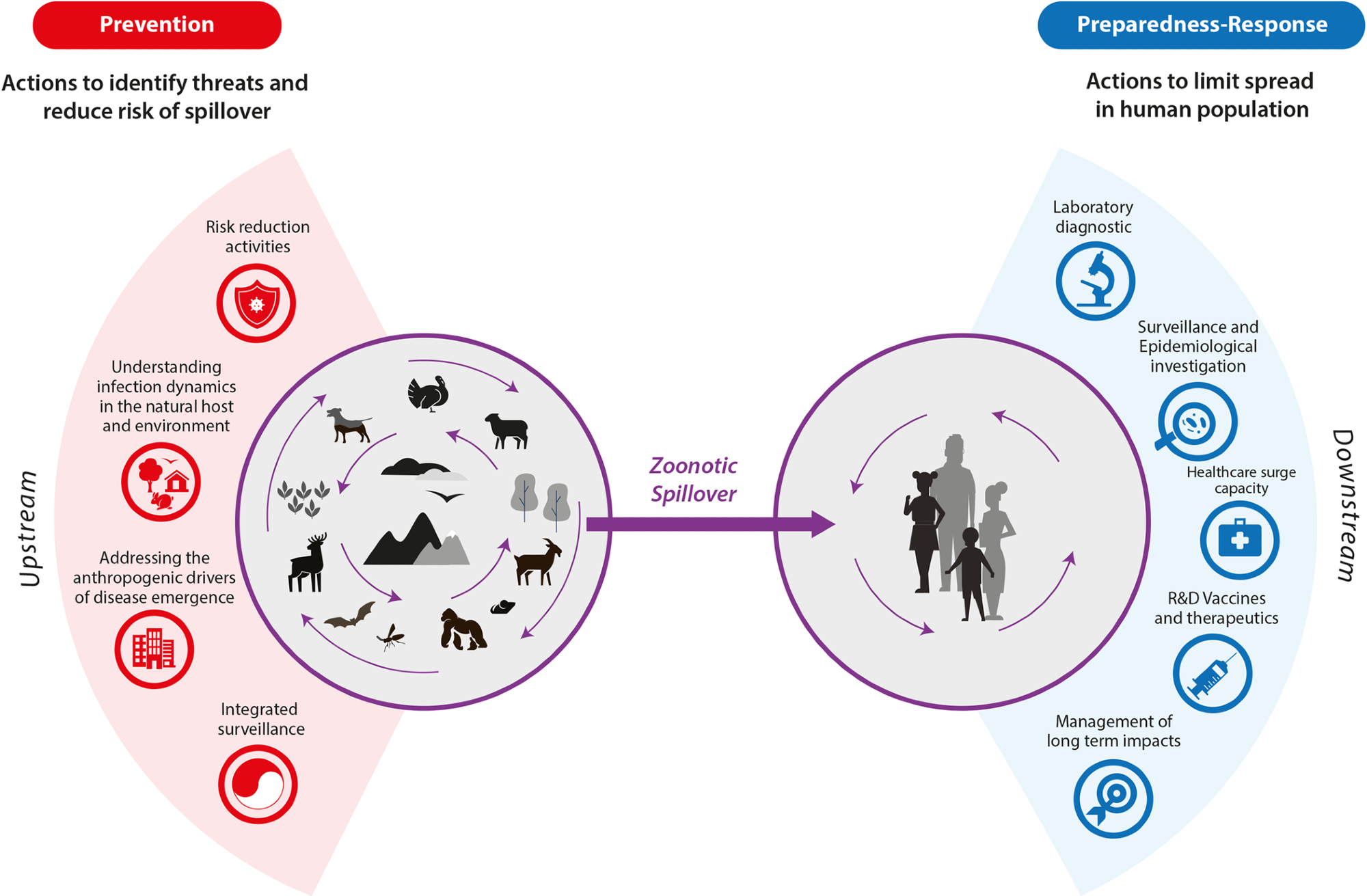
Prevention of zoonotic spillover: From relying on response to reducing the risk at source
One health approach to addressing spillover
A holistic approach to combating spillover can be established by addressing its driving factors through the One Health strategy, which centers on the human-animal-environment nexus. This strategy aims to minimize zoonotic pathogen risks to humans and might incorporate interventions like vaccinations. To provide clarity on priorities for halting future epidemics that could culminate in pandemics, we suggest a definition of prevention concentrated on avoiding zoonotic spillover. This includes all precursor events influencing pathogen spillover, while subsequent activities get categorized as under-preparedness and response actions.
Differentiating primary and secondary prevention
Preventing pathogen proliferation in humans (known as secondary prevention) explicitly pertains to containment strategies activated after the pathogen's introduction to the human populace. These strategies might find applications across various sectors – be it public health, animal health, or environmental management.
Scope of spillover prevention
Fundamentals of spillover occurrence
The foundation of pathogenic spillover from natural sources lies in the direct or indirect contact between humans and the pathogen, usually through an infected host or environment. Importantly, animals and biodiversity are not inherently risky. Instead, it is human actions, which result in risky interactions between species, that amplify spillover probabilities.
The one health approach and identification of risks
Employing a One Health perspective to comprehend the host-pathogen dynamics, such as the pathogen's presence, distribution, evolution, and infection characteristics, can highlight spillover risk factors. Recognizing these risks presents valuable intervention points for spillover mitigation. Although some contexts may demand a multifaceted approach, focusing on prevention has proven to be more economically efficient than solely depending on reactive measures.
Changes in the human-animal-environment interface
Historical and ongoing shifts in the interplay between humans, animals, and the environment offer valuable insights for prevention. Elements like hunting, land use alterations, farming habits, food systems, infrastructural developments, and animal trade patterns are pivotal to formulating preventive strategies. Investing in research that delves into these socio-economic alterations is paramount.
Considerations for vector-borne diseases
Understanding habitat suitability, climatic variables, and host abundance is integral for risk assessment for vector-related illnesses. Even in the absence of pathogen presence and pathogenicity data, recognizing exposure pathways across interfaces can help pinpoint critical control points. Changing human behaviors can reduce infection risks in a broad range of ways.
Determinants of spillover risk
Direct activities like hunting, urbanization, livestock farming with inadequate biosecurity, animal trade, and deforestation influence spillover risk. Additionally, the risk is compounded by overarching factors like climate change, food security, animal and human health concerns, socio-economic disparities, and animal welfare practices. Addressing both direct and broader influencers is essential for holistic spillover prevention.
- Authored by the members of the One Health High-Level Expert Panel (OHHLEP), Markotter W, Mettenleiter TC, Adisasmito WB, Almuhairi S, Barton Behravesh C, et al. (2023) Prevention of zoonotic spillover: From relying on response to reducing the risk at source. PLoS Pathog, 2023, DOI- https://doi.org/10.1371/journal.ppat.1011504, https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1011504
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Biosecurity, CLARITY, Climate Change, Coronavirus, Coronavirus Disease COVID-19, Evolution, Food, Global Health, Health Systems, Infectious Diseases, Pandemic, Pathogen, Proliferation, Public Health, Research, Zoonosis

Written by
Vijay Kumar Malesu
Vijay holds a Ph.D. in Biotechnology and possesses a deep passion for microbiology. His academic journey has allowed him to delve deeper into understanding the intricate world of microorganisms. Through his research and studies, he has gained expertise in various aspects of microbiology, which includes microbial genetics, microbial physiology, and microbial ecology. Vijay has six years of scientific research experience at renowned research institutes such as the Indian Council for Agricultural Research and KIIT University. He has worked on diverse projects in microbiology, biopolymers, and drug delivery. His contributions to these areas have provided him with a comprehensive understanding of the subject matter and the ability to tackle complex research challenges.